Beena Oommen1, Sapna Koju2
1, 2 Associate Professor, ManjunathaCollege of Physiotherapy, Chokkanahalli, Hegdenagar, Bangalore
Mail id: beena2281@gmail.com
ABSTRACT
Background of the study: Stroke is defined by the national institute of neurological disorders and stroke as sudden loss of neurological function resulting from an interference with blood supply to the brain. This study aims to know the effects of very early mobilization on motor recovery following acute stroke.
Methodology: The study was conducted among 40 subjects with acute stroke patient, with modified Rankin scale (MRS) ≥2. The subjects were randomly assigned into two groups equally. Group A (n=20) were given early mobilization which included motor recovery training for 30 minutes and twice in a day within 24-48hours of hospital admission. Group B (n=20) were also given motor recovery training for 30 minutes, twice in a day but only after 72hours of hospital admission. It was done for 6 weeks. Modified Rankin scale, Motor Assessment scale and National institute of health stroke scale pre score was obtained before the intervention and post score after 6 weeks of intervention for both the groups.
Results: The statistical analysis shows that t-value is 1.286 and p-value is 0.206 for modified Rankin scale p>0.05 is statistically not significant. For motor assessment scale t-value is 3.760 and p-value is0.001 hence p< 0.05 it is statistically significant. According to statistical analysis of NIHSS score t-value is 0.931 and p-value is 0.358 with p> 0.05 which is statistically not significant.
Conclusion: There was no significant difference between very early mobilization and mobilization after 72 hours. Sothe study concluded that there may not be helpfulon early mobilization for motor recovery in patient with acute stroke.
Keywords: Stroke, Acute stroke motor recovery, very early mobilization, modified Rankin scale, motor assessment scale, NIHSS.
Received on 25th September 2020, Revised on 16th October 2020, Accepted on 18th November 2020 DOI:10.36678/IJMAES.2020.V06I04.003
INTRODUCTION
Stroke is a leading cause of motor and functional impairments; with 20% of survivors requiring institutional care and 15%-30% being permanently disabled. It affects motor and functional task due to which activities of daily living gets affected. The estimated adjusted prevalence rate of stroke ranges from 84-262/100,000 in rural area and 334-424/100,000 in urban areas. The incidence rate is 119-145/100,000 based on the recent population based studies1-4.
One of the major cause of human morbidity and mortality, it was the sixth leading cause of disability-adjusted year in1990 and is projected to rank fourth by the year 2020.WHO has defined stroke as “a clinical syndrome consisting of rapidly developing clinical signs of focal (or global in case of coma) disturbance of cerebral function lasting more than 24 hours or leading to death with no apparent cause other than vascular origin 5-8. Ischemic stroke is due to cessation of blood supply to the brain and it is the most common type and approximately comprises 87% of the stroke cases. Hemorrhagic stroke is occurs due to rupture of weakened blood vessels in or around the brain tissue9-12.
The effects of stroke can be both physical and mental depend on the site and severity of brain injury. The most common Symptoms of stroke are sudden weakness or numbness of the face, arm, leg, most often on the one side of the body, inability to move, confusion, dizziness, dysarthria, aphasia, visual field defect or sudden loss or blurring of vision, dysphasia, problem with balance and co-ordination and may be loss of consciousness13-19.
Objectives of the Study are to determine motor recovery in patient with acute stroke, to determine the effect of very early mobilization on motor recovery following acute stroke and to determine the effect of early mobilization in stroke.
METHODOLOGY
This is an experimental study with randomized control trial. The study population was patients with acute stroke and conducted at Florence College of physiotherapy and research center, also from neuro-specialist hospital, 80 feet road, Bangalore. Sampling method used in this study was simple random sampling. Sample size for the study was 40 and with a duration of study 6 weeks.
Inclusion criteria: Type of stroke: ischemic or hemorrhagic stroke, Age group: 55-65yrs, Gender: Both male and female, Modified Rankin scale ≤ 2, Acute stroke confirmed on computed tomography scanning, Ability to participate in 30 minutes of physiotherapy sessions.
Exclusion criteria: Early deterioration, Documented palliative treatment, Immediate surgery, Another serious medical illness or unstable coronary condition, No response to voice, Systolic blood pressures lower than 110 mm Hg or higher than220 mm Hg, Oxygen saturation lower than 92% with oxygen supplementation, Resting heart rate of less than 40 beats per min or more than 110 beats per min, Temperature greater than 38·5°C, Aphasia, Cognitive impairment, Severe hemi neglect, Previous history of stroke, Not willing to give consent.
Outcome Measures: Modified Rankin scale, Motor assessment scale, National institute of health stroke scale.
Materials Required: Sphygmomanometer, Pulse Oximetry, Wheelchair, Walker, Splint and braces if needed, Data collection Chart, Consent form.
Permission was taken from the Hospital to carry out the study in acute stroke patient. 40 subjects including both male and female, who fulfilled the inclusion criteria and exclusion criteria, were selected for the study. The information sheet about the study and the consent form were given to the subjects for the approval. Subject’s demographic details such as age, gender, occupation, address, phone number, past history, medical history were documented.
A total of 40 patient aged between 55-65 yrs will be selected out of this 20 patient. Group A received very early mobilization and other half 20 patient. Group B received very early mobilization. They will be mobilized only after 72hrs of onset of acute stroke. Patient was acknowledged about the treatment given and their effect on their activities and prior consent will be taken. Group A, did Very Early Mobilization: The patient will receive early mobilization i.e. mobilization within 24 to 48hr after the onset of acute stroke. It includes active exercise of both upper limb and lower limb followed by side lying, side lying to sitting at edge of bed, standing with and without support, walking and sitting in chair or wheelchair.
Group B, did Mobilization after 72hr received mobilization only after 72hr of onset of acute stroke. This also includes same treatment protocol as group A. i.e. active exercise of both upper limb and lower limb followed by side lying, side lying to sitting at edge of bed, standing with and without support, walking and sitting in chair or wheelchair.
Intervention: Group A (n=20) Very Early Mobilization and the subjects were selected which fulfills inclusion and exclusion criteria. Group A were mobilized within 48hr of onset of stroke. Patient in this group were 1st assessed with the outcome measures i.e. MRS, MAS, NIHSS, then the treatment was started which included were PNF stretching, Passive and active movement to maintain joint integrity and mobility, Bridging, Rolling, Supine to sitting, Sitting with support progressed to sitting without support, Side sitting to check balance of lateral trunk and abductor on one side of body, Sitting to standing supported progressed to unsupported, Standing modified plantigrade, Weight shifting activities transfer weight with feet on the floor, Reach out activities, Walking, with frequency of treatment was once in a day for 6 weeks and duration of training lasted for 30 min per day.
Group B (n=20) mobilization after 72hr. Patients were selected considering inclusion and exclusion criteria. Patient in this group were mobilized only after 72hr of onset of acute stroke. Group B also firstly assessed with all three outcome measures are MAS, MRS, NIHSS and treatment was done which included same as given for Group A, with frequency of once in a day for 6 weeks, Duration of the training lasted for 30 min per day.
Procedure for measuring Modified Rankin Scale (MRS): Patient were assessed with modified Rankin scale which consists of score 0-5 where 0 is no disability and 5 is severe disability patients were assessed with MRS before starting the treatment and after the treatment at end of 6th week.
Procedure for measuring motor assessment sale (MAS): During this examination patient were assessed with motor assessment scale in which each item scored on scale of 1-6 with 8 areas of motor function. Patient were assessed depending upon their motor behavior scoring from 1-6 in which 1 is with maximum assistant and 6 is without assistant. Scoring was done according to performance. It was done before treatment and at the end of 6th week.
Procedure for measuring NIHSS: NIHSS helped to find the severity of stroke, it have 11 different component where 0 shows no any severity in condition and 3 and more shows increasing in severity in condition so patient were asked to perform task according to their performance scoring was done before treatment and at the end of 6th week.
RESULTS
| AGE | GROUP A | GROUP B |
| 55 | 4 | 3 |
| 56 | 2 | 1 |
| 57 | 5 | 4 |
| 58 | 1 | 3 |
| 59 | 1 | 1 |
| 60 | 3 | 2 |
| 61 | 1 | 1 |
| 62 | 1 | 2 |
| 63 | 0 | 2 |
| 64 | 1 | 1 |
| 65 | 1 | 0 |
Table -1: Distribution of subjects with acute stroke according to age in both the groups
The table 1 shows the proportion of subjects with acute stroke according to the age. The age distribution is given as 55 years to 65 years. 55 age group 4 subjects in group A and 3 subjects in group B, 56 age group, 2 subjects in group A and 1 subject in group B. Likewise, age distribution is given for group A and group B.
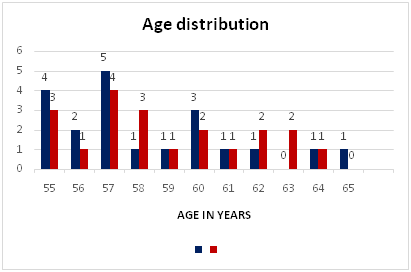
Graph -1: Distribution of subjects with acute stroke according to age in both the groups
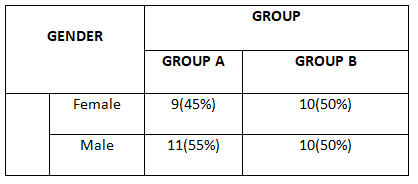
Table -2: Distributionof subjects with acute stroke according to gender in both the groups
The table 2 shows the gender distribution in both the groups in subjects with acute stroke. In group A, 9(45%) of subjects were females and 11(55%) of them were males. In group B 10(50%) were females and 10(50%) were males. There was no much variation in between the groups according to gender and it was found to be statistically not significant at 5% level ie., p>0.05. It evidenced that the subjects with acute stroke according to baseline characteristic of gender is homogeneous in both the groups.
The following bar diagram shows the proportion of subjects according to gender
Graph -2: Distribution of subjects with acute stroke according to gender in both the groups
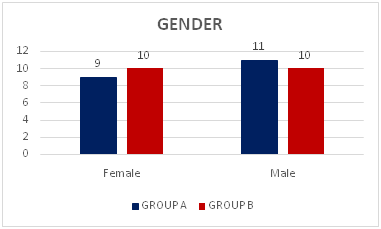
| SIDE | GROUP A | GROUP B |
| LEFT | 8 | 8 |
| RIGHT | 12 | 12 |
Table -3: Distribution of subjects with acute stroke according to body side in both the groups
The table 3 shows the proportion of subjects with acute stroke according to the body side. In group A, 8 subjects affected in left side and 12 subjects were affected in right side. In group B, 8 subjects affected in left side whereas 12 subjects were affected in right side. So, the given subjects were equally distributed in both the groups in the both the sides.
The following bar diagram shows the proportion of subjects according to the side
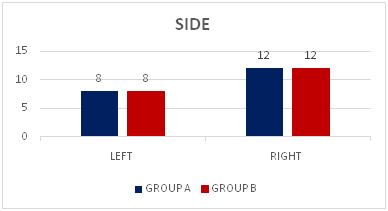
Graph –3: Distribution of subjects with acute stroke according to body side in both the groups
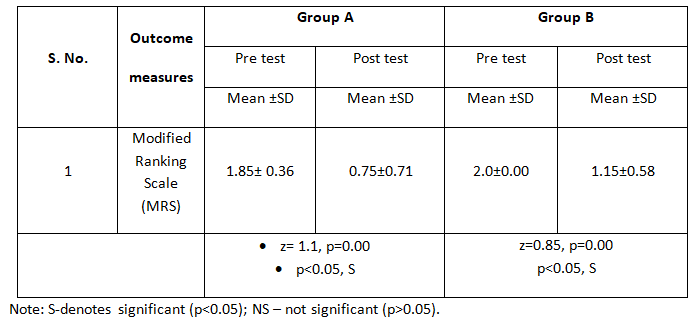
Table-4: Comparison of pre and post test MRS scores among subjects with acute stroke on motor recovery among the groups
The above table -4 shows the pre and post test MRS scores among subjects with acute stroke on motor recovery among the groups. The pre test scores of MRS were 1.85± 0.36 and post test was 0.75±0.71 in group A. The pre test scores of MRS were 2.0±0.00 and post test was 1.15±0.58 in group B.
Pre post comparison in MRS shows that the average improvement is 1.1 in group A with the p value 0.00 and in the group B, average improvement is 0.85 with p value 0.00. Any statistical test is said to be significant if P < 0.05. So it can be notice as post comparison group A is also showing significant improvement and group B also shows significant improvement. So, it can be said as group A and group B is showing significant improvement in MRS.
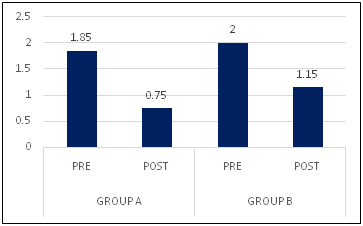
Graph -4: Comparison of pre and post test MRS scores among subjects with acute stroke on motor recovery among the groups
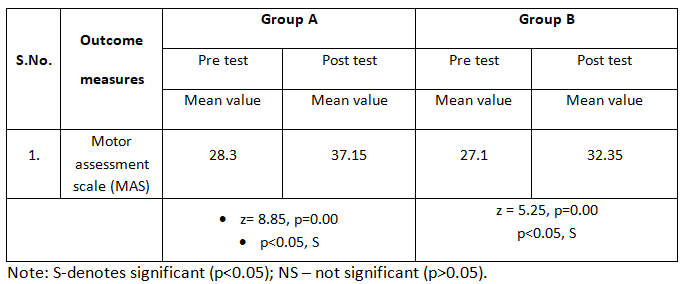
Table-5: Comparison of pre and posttest MAS scores among subjects with acute stroke on motor recovery among the groups
The above table -5 shows the pre and post test MAS scores among subjects with acute stroke on motor recovery among the groups. The pre test scores of MAS were 28.3 and post test was 37.15 in group A. The pre test scores of MAS was 27.1 and post test was 32.35 in group B.
Here, Pre post comparison in MAS shows that the average improvement is 8.85 in group A with the p value 0.00 and in the group B, average improvement is 5.25 with p value 0.00. Any statistical test is said to be significant if (p< 0.05). So, it can be said as group A and group B is showing significant improvement in MAS.
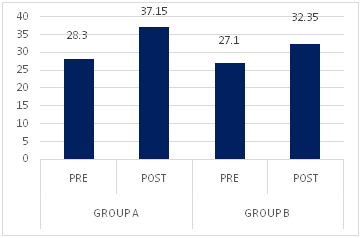
Graph -5: Comparison of pre and post test MAS scores among subjects with Acute stroke on motor recovery among the groups
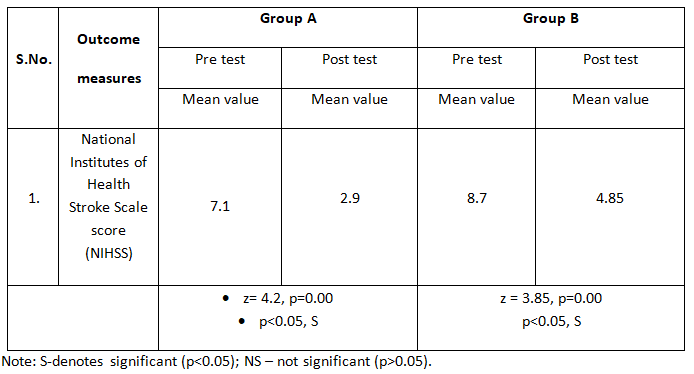
Table 6: Comparison of pre and post test NIHSS scores among subjects with Acute stroke on motor recovery among the groups
The above table -6 shows the pre and post test NIHSS scores among subjects with acute stroke on motor recovery among the groups. The pretest scores of NIHSS were 7.1 and post test was 2.9 in group A. The pre test scores of NIHSS was 8.7 and posttest was 4.85 in group B.
Here, Pre post comparison in NIHSS shows that the average improvement is 4.2 in group A with the p value 0.00 and in the group B, average improvement is 3.85 with p value 0.00. Any statistical test is said to be significant if (p< 0.05). So, it is concluded that there is a significant improvement in NIHSS in the both of the groups.
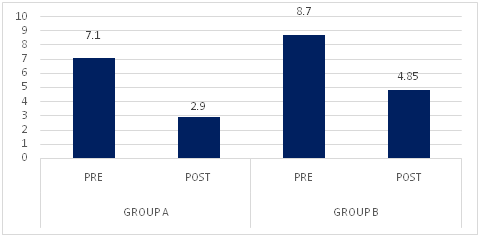
Graph -6: Comparison of pre and post test NIHSS scores among subjects with Acute stroke on motor recovery among the groups
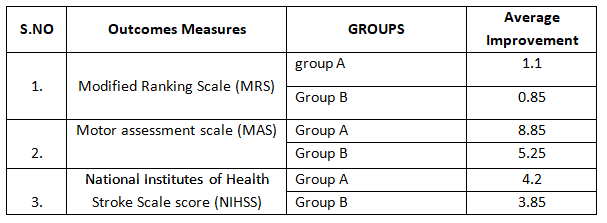
Table 7: Comparison of average improvement of the outcome measures among the subjects with acute stroke in between the groups.
The above table-7 represents the comparison of average improvement of the outcome measures among the subjects with acute stroke in between the groups.
In MRS the average improvement is 1.1 in group A and 0.85 in group B with p value 0.206, which was almost similar and statistically not significant (p>0.05). i.e. both the groups have shown the improvement and equally good.
In MAS the average improvement of 8.85 in group A and 5.25 in group B with p value 0.00,which means there is a significant difference in group A and group B (p<0.05). Therefore, as per the value given Group A is highest so comparatively it shows the good improvement.
NIHSS shows the average improvement of 4.2 in group A and 3.85 in group B with p value 0.358, which is almost similar and statistically not significant (p>0.05) i.e. both the groups have shown the equal improvement.
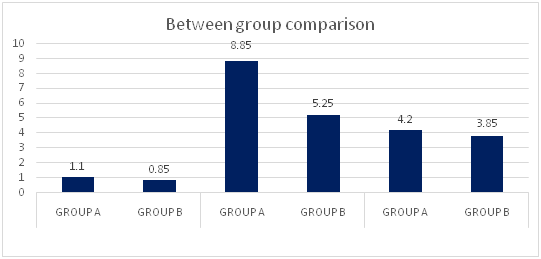
Graph-7: Comparison of average improvement of the outcome measures among the subjects with acute stroke in between the groups.
DISCUSSION
The present study was done to know the effectiveness of very early mobilization on motor recovery following acute stroke. Stroke has been recognized as a common disorder among population. It is a leading cause of motor and functional impairment. Stroke affects motor and functional task due to which activities of daily living gets affected. The effect was evaluated by using MRA, MAS and NIHSS.
This study was conducted among 40 subjects who were randomly assigned into two groups of each group A(n=20) was given very early mobilization which include a set of exercise in lying, sitting and standing followed by walking for 30 minutes. Group B (n=20) was mobilized only after 72hr of onset of acute stroke. Both groups were observed for 6 week.
Out of 40 subjects included in the study 9(45%) were female and 11(55%) were male in group A. In group B 10(50%) were female and 10(50%) were male there was no much variation in between the groups according to gender and it was found to be statistically not significant i.e, it was homogenous in both the groups.
The present study examined the effectiveness of very early mobilization on motor recovery in subject with acute stroke. Pre and post score were evaluated using modified Rankin scale, motor assessment scale and national institute of health science score. Assessment was taken prior to and after the training.
Subject were ranging from 55-65yr, in group A the subject were ranging from 55-65yr with mean and SD 58.3000±2.99297. In group B the subject were ranging from 55-65yr with mean and SD of 58.8500 ± 2.87045. The unpaired t-test was carried to compare the mean which was found to be significant p>0.05. It revealed that the baseline characteristic of age was similar in both the groups.
In the present study Group A very early mobilization shows that pre test modifiedrankin scale mean and SD was 1.8500±.36635. Mean and SD of group B is 2.000±0.000. But in post test group A mean and SD was 7500±.71635. In group B mean and SD is 1.1500±.58714. In comparison to pre and post test group A t-value was 7.678 and p-value is 0.000 i.e P< 0.05 which is statistically significant, this shows that there is significant improvement in motor recovery after acute stroke.
Similarly motor assessment scale (MAS) was also an outcome measure, the MAS shows following statistical values MAS for pre test Group A was mean and SD 28.300±5.56398, post test it was mean and SD 37.15000±7.59692 and group B pre evaluation was mean and SD 27.1000±3.27511 and post evaluation was mean and SD 32.3500±3.97724, t-test and p-test was done to check significance i.e t-value was 10.688 and p-value was 0.000 in group A and in group B t-value was 10.925 and p-value 0.000 here p<0.05 which is statistically significant and shows significant improvement.
NIHSS pre test and post test evaluation score among subjects with acute stroke on motor recovery among the group. The pre test score was 7.1 and post test was 2.9 in group A. the pretest score of NIHSS was 8.7 and post test was 4.85 in group B, here pretest comparison in NIHSS shows that the average improvement is 4.2 in group A with p-value 0.00 and in group B, average improvement is 3.85 with p-value 0.00, any statistical test is said to be significant if p<0.05 so it is concluded that there is a significant improvement in NIHSS in both of the group.
When the comparison of average improvement of the outcome measures among the subject with acute stroke in between group shows, In MRS the average improvement is 1.1 in group A and 0.85 in group B with p value 0.206, which was almost similar and statistically not significant (p>0.05). i.e. both the groups have shown the improvement and equally good.
In MAS the average improvement of 8.85 in group A and 5.25 in group B with p value 0.00,which means there is a significant difference in group A and group B (p<0.05). Therefore, as per the value given Group A is highest so comparatively it shows the good improvement.
NIHSS shows the average improvement of 4.2 in group A and 3.85 in group B with p value 0.358, which is almost similar and statistically not significant (p>0.05) i.e. both the groups have shown the equal improvement.
The study done by Zhumye et al shows similar result that early mobilization done to patient with stroke using barthel index as outcome measure with MRS score ≤2 came to a conclusion that further research is required to verify effect of early mobilization in patient with cute stroke 20,21.
Present study done was also similar to the study done by Torum Askim et al studied to assess motor network changes after ischemic stroke in patient treated with VEM where MRS was less than 3 before admission using mini mental scale examination score shows that there is change in neural activity in relation to the motor learning and motor recovery . So there should be further emphasized in early motor training after stroke 22, 23.
Lindely RL et al also did study in very early mobilization after stroke to know efficacy and safety of the very early mobilization in both hemorrhagic and ischemic stroke where pt were mobilized within 24-48hr was associated with reduction in complication and in odds of favorable outcome gave a conclusion that VEM is effective in practice 24, 25.
Antje S et al research was also similar to the present study which shows that RCT IN very early mobilization in patient with acute stroke has shown improvement in neurological functioning and motor recovery they also had used NIHSS scale to evaluate the improvement in subject 26.
The present study shows that it is statistically not significant so generates an alternative hypothesis i.e very early mobilization on motor recovery after stroke may not shows any improvement during study which is similar to study done by Yelnik P et al that very early active mobility after stroke where patient with acute stroke receives intensive physiotherapy for 45min daily and after study they found that VEM after stroke may not be efficient in impressing motor control 27.
Another study by stott D et al did a pilot RCT in which they found that stroke patient if receive good care in initial days they are more likely to make good recovery and those who receive early mobilization can be benefited and they achieve walking soon without immobilization complication 28.
Above study proves that there may be or may not be an improvement in motor recovery in subjects with acute stroke. While comparison of pre test and post test for motor recovery in acute stroke between the group the pre test score of (MRS) modified rankin scale t-value 1.286 and p-value 2.06 i.e P> 0.05 which is statistically not significant. (MAS) motor assessment scale when compared between the group showed t-value 3.760 and p- value 0.01 which is statistically significant that there was improvement in motor assessment scale in patient with acute stroke. T-value and p- value for NIHSS scale improvement was evaluated where t-value was 0.931 and p-value 0.358, i.e. P> 0.05 which is statistically not significant.
Ethical Clearance: Ethical clearance has obtained from Florence College of Physiotherapy, Bangalore to conduct this study with reference number: FCP/IRB/85,Dated 20/04/2017.
Conflicts of Interest
The author declares that there is no competing interest on conduct of this study and in publishing this article.
Fund for the study: This is self-funded study.
Limitation of study: Sample of the study was limited to a group of 55 to 65 years. Individual learning ability, motivation and cognitive process acts as confounding factors hence may have affected the results. Duration for which the flexibility was maintained post intervention was not studied.
Suggestions & further recommendations: Long-term study can be done. Special attention can be done for the follow–up. Only 40 subjects were obtained. The sample size was small; hence effect seen cannot be generalized.
CONCLUSION
The result of the present study showed that there was no significant difference in the effect of VEM on motor recovery following acute stroke and patient mobilized after 72hrsof onset of stroke. Hence the study accepts null hypothesis and rejects alternate hypothesis. It is concluded that very early mobilization may or may not be helpful for motor recovery in patient with acute stroke.
REFERENCES
- Sunil G. Harsulkar, Keerthi Rao et al: (2013). Effectiveness of Gong‟s Mobilization on shoulder abduction in adhesive capsulitis: A Case Study. Indian Journal of Basic & Applied Medical Research; September Issue-8, Vol.-2, P. 984-989.
- RavinaTaragi, Dr. Siddhartha Sen and Dr. Sonia Khurana (2014). Combined effect of soft tissue mobilization with PNF on glenohumeral range of motion and overhead reach in frontal plane along with pain perception .Int J Advanced Research (2014), Volume 2, Issue 1, 578-586
- SoungYob R, Wi-Young (2014). Analysis of Range of Motion and Isokinetic Strength of Internal and External Rotation According to Humeral Retroversion of the Dominant Shoulder in Youth Baseball Players, Iranian J Publ Health, 43: 178-184.
- Sonakshi Sehgal, Siddhartha Sen, Amit Dhawan (2016). Effects of Muscle Energy Technique in Increasing Range of Motion and Strength of Glenohumeral Internal Rotator, in Athletes with Glenohumeral Internal Rotation Deficit. American Journal of Sports Science. American Journal of Sports Science; 4(2): 43-48
- Burkhart S.S, Morgan C.D, Kibler W.B. (2003).The disabled throwing shoulder: spectrum of pathology, part I: pathoanatomy and biomechanics. Arthroscopy. 19((4)): 404–420.
- Kibler WB Burkhart SS, Morgan CD (2003).The disabled throwing shoulder: spectrum of pathology. Part II: evaluation and treatment of SLAP lesions in throwers. Arthroscopy. 19: 531-539.
- Stephanie D. Moore, Kevin G. Laudner, Todd A. Mcloda (2014). The Immediate Effects of Muscle Energy Technique on Posterior Shoulder Tightness, 2014 Journal of orthopaedic & sports physical therapy; 41: 400-407.
- Michael R. Borich, (2006). Scapular angular positioning at end range internal rotation in cases of glenohumeral internal rotation deficit, J Orthop Sports PhysTher; 36(12): 926-934.
- Jinyoung Lee, Li-Na Kim, Hongsun Song, Sunghwan Kim (2015). The Effect of Glenohumeral Internal Rotation Deficit on the Isokinetic Strength, Pain, and Quality of Life in Male High School Baseball Players, Ann Rehabil Med; 39(2): 183- 190.
- B. Chakradhar Reddy, Santosh Metgud (2014). A randomized controlled trial to compare the effect of muscle energy technique with conventional therapy in stage ii adhesive capsulitis, Int J Physiother Res; 2(3): 549-54.
- Ballantyne F, Fryer G, McLaughlin P. (2003). The effect of muscle energy technique on hamstring extensibility: the mechanism of altered flexibility. J Osteopath Med., 6: 59-63.
- Kevin G Laudner, Robert C Sipes, and James T Wilson, (2008). The Acute Effects of Sleeper Stretches on Shoulder Range of Motion. Athl Train., 43(4): 359–363.
- Jakson K joseph, Sunish A.V. (2013). The Immediate Effects of Sleeper Sretches on Shoulder Range of motion in Volleyball Players. Innovative Journal of Medical and Health Science 3: 4 ; 171 – 176.
- EdrishSaifee Contractor1, Dhara Santosh Agnihotri, Ronak Mukeshbhai Patel (2016). Effect of Spencer Muscle Energy Technique on pain and functional disability in cases of adhesive capsulitis of shoulder joint. IAIM, 3(8): 126-131.
- D L Falla, S Hess, C Richardson (2003). Evaluation of shoulder internal rotator muscle strength in baseball players with physical signs of glenohumeral joint instability, Br J Sports Med; 37: 430–432.
- Cools A M, Johansson FR, Cagnie B, Cambier DC, Witvrouw E E. (2012). Stretching the posterior shoulder structures in subjects with internal rotation deficit: comparison of two stretching techniques. Shoulder & Elbow ;4(1):56–63.
- Richa Mahajan, Chitra Kataria, Kshitija Bansal (2012). Comparative effectiveness of Muscle Energy Technique and static stretching for treatment of subacute mechanical neck pain, International Journal of Health and Rehabilitation Sciences; 1 (1): 16-23.
- Myers JB, Laudner KG, Pasquale MR, Bradley JP, Lephart SM. (2006). Glenohumeral range of motion deficits and posterior shoulder tightness in throwers with pathologic internal impingement. Am J Sports Med. 34: 385-91.
- Moore SD, Laundner KG, Mcloda TA, Shaffer MA. (2011). The immediate effects of muscle energy technique on posterior shoulder tightness: a randomized controlled trial. J Orthop Sports PhysTher. 41(6); 400-7.
- Aldridge R, Guffey JS, Whitehead MT, Head P. (20120. The effects of a daily stretching protocol on passive gleno humeral internal rotation in overhead throwing collegiate athletes. Int J Sports PhysTher; 7(4): 365-71.
- MitChell UH, Myrer JW, Hopkins J, Hunter I, Feland JB, Hilton S C. (2007). Acute stretch perception alteration contributes to success of the PNF “contract-relax” stretch. J Sports Rehabil; 16: 85-92.
- M. Seshagiri Rao, Swathi Tejitha (2016).Comparison of 3 stretching protocols for posterior shoulder tightness in throwers. International Journal of Physiotherapy and Research, Int J Physiother Res Vol 4(2):1429-35.
- Juneja H, Verma, S. K., Khanna (2011). Isometric Peak Force of Shoulder Rotators in Cricketers with and without History of Shoulder Pain, Journal of Exercise Science and Physiotherapy; 7 (1): 42-49.
- Jacquelyn M. Downar; Eric L. Sauers, (2005). Clinical measures of shoulder mobility in the professional baseball player, Journal of Athletic Training; 40(1): 23–29.
- Leandro Anonietti, Natalia Luna, Gabreil Nogueira et al., (2014). Reliability Index of inter- and intra-rater of manual goniometry and computerized bio-photogrammetry to assess the range of motion of internal and external shoulder rotation, Medical express; 1(2): 95-99.
- Mark G Grossman MG, A Cadaveric Model of the Throwing Shoulder (2005). A Possible Etiology of Superior Labrum Anterior-to- Posterior Lesions, J Bone Joint Surg Am; 87 (4): 824-831.
- Donatelli R, Ellenbecker T.S, Ekedahl S.R, Wilkes J.S, Kocher K, Adam J. (2000). Assessment of shoulder strength in professional baseball pitchers. J Orthop Sports Phys Ther. 30 (9) : 544–551.
- Manske RC, Meschke M, Porter A, Smith B, Reiman M. (2010). A randomized controlled single-blinded comparison of stretching versus stretching and joint mobilization for posterior shoulder tightness measured by internal rotation motion loss. Sports Health. 2: 94-100.
Citation:
Beena Oommen, Sapna Koju (2020). Effects of very early mobilization on motor recovery following acute stroke- A randomized control trial, ijmaes; 6 (4); 854-868.

Leave a Reply