| Syeda Khanam. P1, Manjunatha. H2, Thummala S. Pavani3 |
Corresponding Author:
1Professor, East College of Physiotherapy, Bidrahalli, Bangalore, Karnataka, India
Co Authors:
2Principal, East College of Physiotherapy, Bidrahalli, Bangalore, Karnataka, India
3Assistant Professor, East College of Physiotherapy, Bidrahalli, Bangalore, Karnataka, India
ABSTRACT
| Background and purpose: This study was to find the effect of inspiratory muscle training on dyspnoea and exercise tolerance among chronic obstructive pulmonary disease patients. Methods: It is a randomized control study of 30 COPD participants with 15 in each control and experimental group. Experimental group underwent inspiratory muscle training with threshold IMT device in the physiotherapy department, where subjects have to breathe against various threshold levels, 30sets/sessions where as control group underwent only breathing and general mobility exercises at home. The training lasted for 20-30 minutes, twice daily 6days per week, and was continued over the course of 4 weeks duration. Parameters included were 6minutes walk test, MRC dyspnoea grade, PEFR values. The data collected data of control and experimental group was compared to find the outcome. Results: Before interventions, all patients showed increased dyspnoea levels and reduced exercise tolerance. After interventions they all exhibited reduced dyspnea and increased exercise tolerance based on 6min walk test, MRC dyspnoea grade, PERF Parameters. Control group patients didn’t exhibit any improvement in any of the parameters. Conclusion: The results support that inspiratory muscle training is more effective on reducing dyspnoea and increasing exercise tolerance among COPD patients. Keywords: Chronic Obstructive Pulmonary; Dyspnoea; Exercise tolerance; Inspiratory muscle training |
| Received on 20th January 2021, Revised on 4th February 2021, Accepted on 24th February 2021; DOI:10.36678/IJMAES.2021.V07I01.003 |
INTRODUCTION
Chronic obstructive pulmonary disease is a condition characterized by narrowing of airway tract with symptoms of chronic cough, expectoration, wheeze and exertion dyspnoea. COPD can develop and progress by 25% risk factors of smoking and to mortality by 15% with addiction of smoking 1-3.
Diaphragm is the main inspiratory muscle morphologically and functionally responds to the inspiratory muscle training. There are evidence documented in possibility of resultant accumulation of co2 takes place even after resolution of acute exacerbation of conditions and relative obstruction of airway 4, 5.
The IMT device can help to do inspiratory training exercise which can increase strength of inspiratory muscle; there by it can improve the threshold of inspiratory resistance. Overall health related quality of life (HRQL) can improve by repeated inspiratory muscle training. The exercise training decrease dyspnoea and work of breathing becomes easier in patients with COPD. Regular inspiratory training can facilitate to perform physical activities more easily 6-10.
Aims and objectives of the study was to find the effect of inspiratory muscle strength and endurance to increase exercise tolerance, decrease work of breathing, and to improve functional exercise capacity and also to increase overall health related quality of life.
METHODOLOGY
The study Design was Randomized control study. Data collected were from the patients recruited from pulmonology OPD and treated in the physiotherapy department, Nizam’s institute of medical sciences, punjagutta Hyderabad. Patients were assessed thoroughly and treated during the trails. Period of study intervention was 4 weeks and materials used were threshold inspiratory muscle trainer.

Peak expiratory flow meter is used to record the peak expiratory air flow rate of a person. The forced expiratory volume of a person is measured using this device. The forced expiratory volume of a person is measured using this device. The forced expiratory volume is given in liters’/minute. In COPD patients the PEFR is altered due to biomechanics of chest.
GAIAMS*Power breathe provides a threshold resistance during inspiratory phase. It helps in increasing strength and endurance of respiratory muscles, reduce severity of dyspnoea and improves exercise capacity patients with COPD, asthma, cystic fibrosis, chronic heart failure,chronic spinal injury, muscular dystrophy, before cardio thoracic surgery.Materials required for the study was Sphygmomanometer, Stop watch, and Measure tape 11-14.
It has got 9 levels and load varies from level 1 to level 9, approximately as follows: Load (-cm H2O).
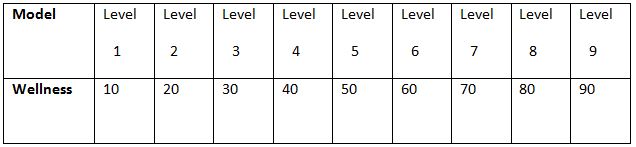
Intensity: 10% to 52% of maximal inspiratory pressure (PI Max).most commonly used training device in these studies is threshold IMT. Frequency of the study duration was 7days/week and total duration of the study was 4 weeks, 20-30 min session, twice a day.
Procedure: Subject has to sit in a high sitting position on a couch, hold the apparatus close to the mouth and take deep breathe against the resistance set with in the threshold IMT apparatus and blow air out relax. Patient has to repeat the same for 30 times. This procedure should be done twice a day, 30 minute every session. Patient is instructed properly and to discontinue usage if they have symptoms of breathlessness and cough.

Inclusive criteria for this study was Mild and moderate exacerbation of COPD
Exclusive criteria for this study was Severe exacerbation of COPD, Pulmonary tuberculosis, Restrictive lung disease, Severe asthma, neuro muscular disorders, musculo skeletal problems of spine, Heart failure/unstable angina and Peripheral vascular diseases.
The data collected ranged from parameters: 6 min walk test, Peak expiratory flow rate, and MRC dyspnoea grading.
During study period 60 patients were examined who were all COPDS associated with other problems but only 30 met the inclusive criteria.15 patients were assigned for group A and remaining 15 for group B according to randomized control study. Their mean ages (group A 58.13; group B 52.06) were calculated.
Data analysis and results: All data analysis was computed with statistics, paired T-test .within groups, student T-test between groups and mean values were used for both groups to determine the difference between outcome measures of 6 min walk test, MRC dyspnoea and PEFR. Level of significance was fixed as 5 % for the present study.
Out of large proportion COPD with mild and moderate exacerbation the sample taken for the study is 30,based on convenience sampling method after thorough examination based on inclusive criteria from the department of physiotherapy.30 participants were present for the whole duration of the study 4 (week).
During 4 week of study course the parameters studied were 6 min walk test, MRC dyspnoea scale, Peak expiratory flow rate.
The data was collected on subject on 1st week and 4th week, and raw data was arranged in order to maintain the master chart, which was subjected to further statistical analysis.
To find out of the average line score in above mentioned parameters in each subject the means were calculated at 1st week and these values were considered as base line values for the study simultaneously the same parameters are studied at 4th week and average variations were recorded in terms of means of each parameters and the variations from the mean were also calculated.
The difference in each parameter from 1-4 weeks was tested with paired T-test, within group and student T-test between groups, finally the observed variations in each parameter was represented in graphical format for easy understanding.
RESULTS
From 1st week to 4th week all the parameters collected from the data are arranged in master chart for further statistical analysis .The difference in each parameter from 1st week(initial )to the end of 4th week(final),of the subject is shown in the following tables.
6 Min Walk Test: The performance of 6min walk test was conducted for both the groups (Experimental and control group) that to in particular time schedule (1st week to 4th week). 1st week taken as base period which is compared with other time factors, combination allay. Different variables were studied between: 1st week-4th week. For with group paired T-test was performed and among two different groups student T-test was used; same tests are used for other parameters MRC dyspnea, PEFR too.
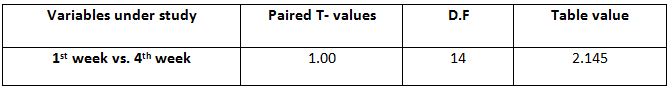
Within Control Group: Among all the variables within the control group, paired T-test calculated value for 1st -4th week is 1.00000 and the table value is 2.145 at 5%level of significance with 14 degrees of freedom.
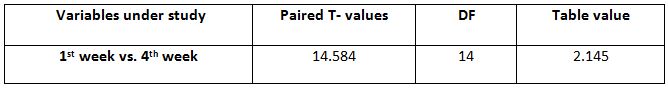
Within Experimental Group: Among all the variables within the experimental group, paired T –test calculated value for 1st week -4thweeks is 14.58441 and the table value is 2.145 at 5% level of significance improvement in 6minute walk in experimental group to control
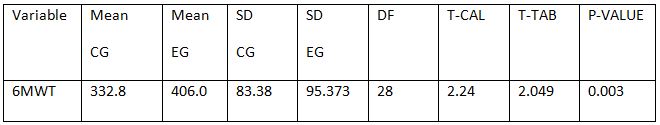
Between Control Group and Experimental Group: Between control and experimental group student T-test was performed. Among all the variables the student T- test calculated values for 1st and 4th week (2.24).
The tabulated value at 5% level of significance with 28 degree of freedom is 2.049 showing the significant difference.
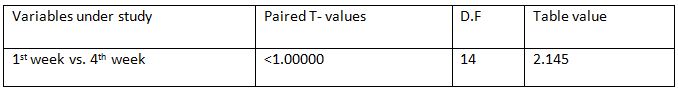
MRC Grading of Dyspnea within Control Group: Among all the variables with in control group, paired T-test calculated value for 1st week-4th week is less than 1.000 and the Table value is 2.145 at 5%level of significance with 14 degrees of freedom.
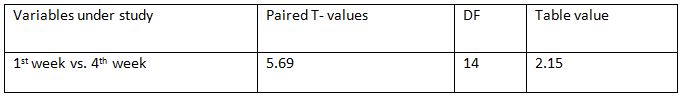
MRC Grading of Dyspnea within Experimental Group: Among all the variables within the experimental group, paired T –test calculated value for 1st week -4th weeks is 5.69 and the
table value is 2.15 at 5% level of significance improvement in dyspnoea levels in experimental group to control
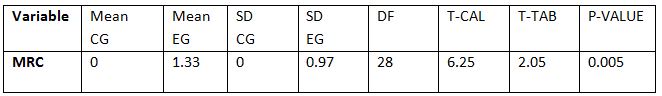
MRC Grading of Dyspnea between Control Group and Experimental Group: Between control and experimental group student T-test was performed. Among all the variables the
student T- test calculated values between1st and 4th week (6.25).The tabulated value at 5% level of significance with 28 degree of freedom is 2.05 showing the significant difference.
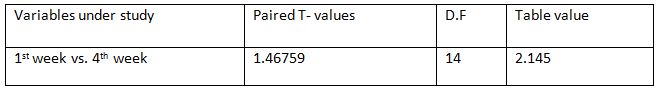
Peak expiratory flow rate within Control Group:Among all the variables within the control group, paired T-test calculated value for
1st -4th week is 1.46759 and the table value is 2.145 at 5%level of significance with 14 degrees of freedom.
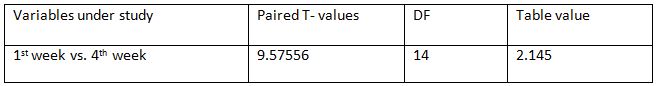
Peak expiratory flow rate within Experimental Group: Among all the variables within the experimental group, paired T –test calculated value for 1st week -4th weeks is 9.57556 and the
table value is 2.145 at 5% level of significance with 14 degrees of freedom showing significant improvement in PEFR values in experimental group compared to control
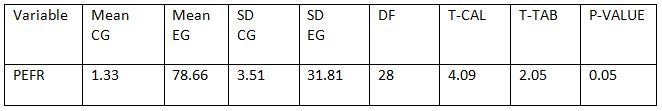
Between Control Group and Experimental Group: Between control and experimental group student T-test was performed. Among all the variables the student T- test calculated values for 1st and 4th week (4.09).The tabulated value at 5% level of significance with 28 degree of freedom is 2.05 showing the significant difference.
DISCUSSION
COPD is progressive and irreversible disorder of airway. Therefore even after resolution of acute exacerbation of condition there may be relative obstruction of airway. So complete expiration is not possible after resultant accumulation of Co2. Therefore, these patients frequently report dyspnoea related to activities of daily living, such patients are considered as stable COPD patients. The symptom induced inactivity leading to deconditioning and muscle weakness & thus resulting into crucial impact of functional and health status15-17.
The present study has done on patients with mild and moderate COPD for 4 weeks showed significant effects of IMT on dyspnoea &exercise tolerance. Many studies have reported the effect of inspiratory muscle training on dyspnoea and exercise tolerance among COPD Patients. Parameters included in this study are 6 minute walk distance test, PEFR, and MRC grading of dyspnoea.
In experimental group in present study the mean improvement in 6 minute walk distance at the end of 4 weeks of training is 109.4 m, T cal values 14.584, T tab value 2.145, showing significant improvement. In control group the mean difference in 6 min walk is 3.2 m at the end of 4th week T cal values 1.000, T tab value 2.145, showing no significant improvement. The limiting factors for reduced exercise tolerance in patients with COPD are dyspnoea. The increase in 6 min walk distance could be because of reduction in dyspnoea, increased exercise tolerance.
PEFR mean difference within the experimental group is78.66 T cal values at the end of 4th week is 9.576 and the, T tab value 2.145, showing significant improvement compared to control group where the mean difference is 1.33, T cal values 1.468, T tab value 2.145. MRC grading of dyspnoea within experimental group at end of 4th week the mean difference is 1.33, T cal values 5.69, T tab value 2.15, showing significant changes in dyspnoea levels in experimental group compared to control where there is no significant changes in mean values, at the end of 4th week T cal values is less than 1.000, and T tab value is 2.145.
A study on specific inspiratory and specific expiratory muscle training has proved both are effective on improving respiratory function, specifically it could reduce dyspnoea and improve exercise performance. There was no difference in effect on the outcomes when the patient performed combined specific inspiratory and expiratory muscle training exercise program among COPD Patients 18-20.
The effect of specific expiratory muscle training for one year among COPD patients have shown, it improves in respiratory muscle strength and health related quality of life. The study has also reported maximal inspiratory pressure and improves 6 minute walk distance and a decrease in the mean Borg score during breathing against resistance scores. Some studies have reported inspiratory muscle training has improved functional exercise capacity and strength of respiratory muscles 21, 22.
Present study even showed significant improvement in dyspnoea, exercise tolerance in COPD who underwent IMT for 4 weeks. Most commonly used training device in these studies is threshold IMT where intensity varied from 10% to 52% (high) of maximal inspiratory pressure (PI max) 20-30 min session, twice a day.
The reduction in dyspnoea due to IMT could be due to increased inspiratory muscle strength as determined 20% Larson et al. study (1999), 34% Lisboa et al(1997), 25%weiner et al (2000),50%, Sachez Riera et al (2016).
Inspiratory muscle training for five weeks has proved effect on external intercostals muscles with strong evidence of biopsy report on increase in size of type 2muscle fibers among COPD patients.
A study among COPD patients in Spain, they have analyzed health related quality of life (HRQL) using Questionnaire after inspiratory muscle training and found effect on outcomes of sustained maximal inspiratory pressures, shuttle walk test, in experimental group.
Comparatively the present study even showed significant changes and improvement in dyspnoea and exercise tolerance on mild and moderate COPD patients where the duration of the study was for 4 weeks and the outcome measures used were 6 min walk test, MRC dyspnoea grade and PEFR values. Experimental group showed significant improvement in all these outcome measures than the control group.
In a study conducted at south Korea, the effects of inspiratory muscle training has reported the changes in outcome measures of FEV1, level of dyspnoea based on Borgs score, and 6 min walk distance, they were analyzed in experimental group and showed decreased perception of dyspnoea and improved exercise capacity among moderate to severe obstructive components in the presentation of COPD.
Comparatively in the present study subjects were only mild, moderate COPD patients where control group did not participate in IMT for 4 weeks but practiced general mobility exercises and breathing exercises where as experimental group who underwent inspiratory muscle training showed significant improvement in dyspnoea and exercise tolerance.
The meta-analysis has reported the effect of inspiratory muscle training on inspiratory muscle strength and endurance, improved functional exercise capacity and decreased dyspnoea in patients with COPD. The documented effects of inspiratory muscle training were examined in a meta-analysis. The study is also recommended inspiratory muscle training is a very essential addition to pulmonary rehabilitation programs.
In the present study done on patients with mild and moderate COPD for 4 weeks the experimental group showed significant effects of IMT on dyspnoea &exercise tolerance than control group who underwent only breathing and general mobility exercises.
The studies conducted were performed on a limited number of subjects. Further study is required on a large group to quantitatively analyze the results of IMT on large scale.
Ethical Clearance: Ethical clearance has obtained from Faculty of Physiotherapy, Nizam’s Institute of Medical Sciences, Punjagutta, Hyderabad on 02/05/2008 to conduct this study.
Conflict of interest: There was no conflict of interest to conduct this study.
Fund for the study: It was aself financed study.
CONCLUSION
The study has concluded from the study that inspiratory muscle training can reduce dyspnoea and improved exercise tolerance in COPD patients with mild and moderate exacerbation. The study has also supported the exercise program can improve overall health related quality of life (HRQL) among COPD patients.
Limitations: Limitations of the study were small sample size, short time training period, IMT apparatus is not accessible and it is cost effective for the patients and study was limited to a specific group of mild and moderate COPD.
Future Direction: The present study can be extended for long term rehabilitation. Future study can imply IMT on severe exacerbation of COPD/chronic asthma, cystic fibrosis, pre op lung conditions such as lobectomy, pneumonectomy. Pre and post training PI Max value of IMT can be taken to further strengthen the study, and also can imply expiratory muscle training.
REFERENCES
- Nice, L (2000). Mechanism and measures of exercise intolerance in chronic obstructive lung disease.Clin Chest Med 21, 693-704.
- Van’tHul, HA, Gosselink, R, Kwakkel, G (2003). Constant-load cycle endurance performance; Test-Retest reliability and validity in patients with COPD. J Cardio-pulmo rehabil. 143-150.
- Polkey, MI, Moxham, J, (2004). Improvement in volitional tests of muscle function alone may not be adequate evidence that inspiratory muscle training is effective Eur Respir. J, 23, 5-6.
- Holm, P, Sattler, A, Fregosi, RF (2004). Endurance training of respiratory muscle improves cycling performance in fit young cyclists.BMC Physio., 4: 9.
- Weiner, P, Magadle,R, Beckerman, M, et al (2003). Specific expiratory muscle training in COPD. Chest 124, 468-473.
- Weiner, P, Magadle, R, Beckerman, M, et al (2003). Comparison of specific expiratory, inspiratory and combined muscle training program in COPD Chest 124, 1357-1367.
- Bourjeily, G, Rochester, C L, (2000). Exercise training in chronic obstructive pulmonary disease, Clinical chest med, 21,763-781.
- Caine MP and MC Connell AK (2000). Development and evaluation of a pressure threshold inspiratory muscle trainer for use in the context of sports performance. Sports Engin 3,149-159.
- Covey MK, Larson JL, Wirtz SE, Berry JK, Pogue NJ, Alex CG and Patel M., (2001). High intensity inspiratory muscle training in patients with chronic, obstructive pulmonary disease and severely reduced function. J. Cardiopul. Rehabil. 21; 231-240.
- Lotters, F, Kwarkkel, G, Gosselink, R. (2002). Effect on controlled inspiratory muscle training in patients with COPD.A Meta-analysis. European Respiratory Journal, 20,570-577.
- Oh, Eui-Geum. (2003).The Effect of home-Based pulmonary Rehabilitation in patients with chronic lung disease. International journal of nursing studies, 40, 873-880.
- Beckerman, Marinella, Magadle, R, (2005, November). The effect of one year of specific inspiratory muscle training in patients with COPD. Chest, 5, 3177-3183.
- Martin, Daniel, (2002). Use of inspiratory muscle strength training to facilitate ventilator weaning. Chest 122,192-196.
- Sanchez, RH, Monte mayor, RT, Ortega, RF, et al. (2001). Inspiratory muscle training in patients, with COPD; Effect on dyspnoea, exercise performance, and quality of life chest 120,748-756.
- De Jong W, Van Aalderen WM, Koeter GH, and van der schans CP.(2001). Inspiratory muscle training in patients with cystic fibrosis. Respir Med., 95: 31-36.
- Enright, S, Chatman, K, Lonescu, A.(2004). Inspiratory muscle training improves lung function and exercise capacity in adults with cystic fibrosis. Chest, 2, 405-412.
- Lisobia, C, Munoz, V, Beroza, T, Leiva, A, Cruz, E, (1994). Inspiratory muscle training in chronic airflow limitation: A compensation of two different training loads with a Threshold Device European Respiratory Journal, 7, 1266-1274.
| Citation: Syeda Khanam. P, Manjunatha. H, Thummala S. Pavani (2021). Effect of Inspiratory Muscle Training in Patients with Chronic Obstructive Pulmonary Disease on Dysponea and Exercise Tolerance, ijmaes; 7 (1); 933-942. |

Leave a Reply