| Deepthi. RNV 1, Daranisri J2, Jibi Paul3 |
| Authors: 1Assistant professor, Faculty of Physiotherapy, Dr. MGR Educational and research institute University, Chennai, Tamilnadu, India 2BPT, Faculty of Physiotherapy, Dr. MGR. Educational and research institute University, Chennai, TN, India 3Professor, Faculty of Physiotherapy, Dr. MGR. Educational and research institute University, Chennai, TN, India Corresponding Author: 1Assistant professor, Faculty of Physiotherapy, Dr. MGR Educational and research institute University, Chennai, Tamilnadu, India, Email id: deepthirnv@gmail.com |
ABSTRACT
| Background: Anorectal pain is a manifestation of several structural and functional disorders affecting the anus and rectum, urinary bladder, reproductive system and pelvic floor musculature. Aim and objective of the study: to determine the effect of pelvic floor muscle training (PMFT) and anal self-massage to improve quality of life in women with anorectal pain. Objective of the study is to improve pelvic floor muscle strength by using PFM training. Anal self-massage to treat the anal fissure and improve the quality of life in women with anorectal dysfunction. Methodology: An experimental study with thirty parous women with anorectal pain was taken using pre and posttest who meet the criteria of realize scoring scale and also, they included in the inclusion criteria are, age group 25 – 45 years of parous women, patients with anorectal pain, fecal incontinence, anal fissure, acute hemorrhoids, and excluded by the exclusion criteria of chronic hemorrhoids, age group above 50 years of women, un willing patients. and at the end of the study the posttest was taken, then comparing the effectiveness of treatment among the groups. Outcome Measures were rectal pain scale, oxford pelvic grading scale, realise scoring scale. Result: PFMT along with anal – self massage found more effective for anorectal pain than anal – self massage and PFMT in anorectal pain with a mean difference of p<0.001 among women with anorectal pain. Conclusion: by the result obtained from this experimental study, PFMT along with anal – self massage found to be more effective than anal – self massage and PFMT among women with anorectal pain. Keywords: Norectal pain, Pelvic floor muscle training, Rectal pain scale, Anal self-massage, Realize score |
| Received on 19th February 2024; Revised on 25th February 2024; Accepted on 29th February 2024. DOI:10.36678/IJMAES.2024.V10I01.005 |
INTRODUCTION
Anorectal pain is a manifestation of various functional and dysfunctional effects on the anus, rectum, bladder, reproductive system and abdominal muscles. Anorectal pain has many causes, including hemorrhoids, anal fissures, and trauma. This is a common proctological problem associated with poor lifestyle. Basic knowledge of pelvic floor anatomy and physiology is essential to understanding the causes of anorectal pain1,2. The pelvic floor is a muscular diaphragm that supports the intestines, leaving the space for the anus, vagina, and urethra into the perineum. The levator ani is the most important muscle and it includes four muscles they are pubococcygeus, puborectalis, lliococcygeus and coccygeus.
The puborectalis surrounds the anus before it enters the pubic bone and can be palpated by examining the pelvic floor3,4. The action of the striated muscle is shared by the external rectal sphincter. Unlike diseases such as endometriosis, pelvic pain is a dysfunction that cannot be explained by the process or other pathological processes. Dysfunction was classified as anorectal (eg, rectal pain, levator ani syndrome, and otherwise unspecified pain), bladder (eg, interstitial cystitis (IC) or bladder pain urinating)4,5,6. The incidence of anorectal symptoms increased from 9.4% to 21.2%.7% the current study shows that the frequency of female patients is higher than that of male patients. According to varadarajan MS.et.al among 325 patients from tamil nadu (India) with anorectal aliments, 100 patients (30.7%) has anal fissure of these 54 patients were males and 46 were females were affected by this issues16. The prevalence of anal fissure among patients with anorectal complaints is around 18%. Mixed dietary habits constipation could be considered as risk factors for the anal fissure, anorectal disorder including hemorrhoids, inflammatory bowel disease among common population.
Proctalgia fugax (PF) the term suggests condition characterized by sudden, severe pain in the anal canal or low rectum. The prevalence of this issue is about 8% to 18% of women between the ages of 30 to 50 years. The levator ani syndrome and proctalgia fugax both are asymptomatic during rectal examination and there are no characteristic physical findings to support the diagnosis, which is based on the clinical description and the exclusion of anorectal diease producing rectal pain, even if palpation of the puborectalis muscle allows the exact localization of the symptom. The distinction between the different groups of perineal pain is based solely on the patient’s description of the pain and location of tenderness by palpation.
Pelvic Floor Muscle Training (PFMT): pelvic floor muscle training which helps in strengthen the muscles under the uterus, bladder, bowel and the muscles of the pelvic floor13. It is very important to relaxing the abdominal, buttocks, deep anal sphincter muscle and thigh muscle along while doing PFMT. Can also strengthen these muscles by using a vaginal cone, which is a weighted device that is inserted into the vagina. Then doing the PFMT to strengthen by contracting and relaxing the pelvic floor group of muscles14,15.
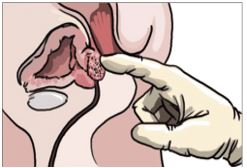
Figure 1 Anal Self – Massage
Anal Self-Massage: It is a method to treat anorectal pain with a finger that appears to induce a better resolution of anorectal pain than anal dilators. Through anal self-massage, the patient modulates the action of dilating, making the therapy more effective and performing real biofeedback18.
Aim of The Study: The aim of the study is to find the effectiveness of PFMT along with massage to enhance muscle strength and quality of life women with anorectal pain
Need Of the Study: PFMT is used to improve the pelvic floor muscle strength and tone Anal-self massage is used to reduce pain in the anal surface and relaxing the area to improve and enhancing the quality-of-life o women with anorectal pain. This study is an attempt to see the effective of PFMT along Anal-self massage in women with anorectal pain.
METHODOLOGY
This is a comparative experimental study conducted at ACS medical college and hospital, Velappanchavadi, chennai-77. Sample size of 30 subjects selected for this study andSimple sampling method used to allocate the samples in three groups. This study conducted for duration of 6 weeks.
Inclusion Criteria: Age group 21-45 years of parous women, Patients with anorectal pain, Fecal incontinence, Anal fissure, Acute hemorrhoids.
Exclusion Criteria: Chronic hemorrhoids, Age group above 50 years of women, Un willing patient, Active Infection, Osteotomy surgery, Anal rectal stenosis, Imperforate anus, Stricture
Material Used were Couch, Lubricant gel and gel ball.
Outcome Measure were Quality of life and Anal muscle strength (Ano-rectal squeeze test).
Measurement Tools were oxford pelvic grading scale, Rectal pain scale and Realise score.
Independent variables: Pelvic floor muscle training (PFMT) and Anal self-massage.
Procedure: Thirty women with anorectal pain were randomly assigned after the pretest for the treatment of pelvic floor muscle training (PFMT) and anal self-massage. Subjects included were age group 25 – 45 years of parous women, patients with anorectal pain, anal fissure, constipation, acute haemorrhoids, and excluded those with chronic haemorrhoids, age group above 50 years of women, unwilling patients, any pelvic floor or vaginal infection. A detailed explanation about the treatment protocol was given to the patient’s, Informed consent was collected and they were selected by a simple random sampling method-lottery method.
The subjects were divided into Group A, Group B, Group C. Subjects were assessed by Realise score, oxford pelvic floor grading scale and pain was assessed by rectal pain scale and pretest measurement will be taken. All patients will receive the intervention for 6 weeks and be evaluated at baseline and after 6 weeks. After the session was complete, subjects were post-tested and recorded using the Realise score, Oxford Pelvic Floor Rating Scale, rectal pain scale.
We analyzed and interpreted the recordings and recorded the results. 10 people in group A received PFMT, 10 people in group B performed anal self-massage, and 10 people in group C performed both PFMT and anal self-massage. All patients will be evaluated at baseline and with follow-up testing after 6 weeks. Pain was measured using rectal pain scale. Patients are required to complete a consent form and two validated questionnaires at baseline. We quantified mean pain intensity during defecation and measurement of pain intensity, graded from 0 (no pain) to 10 (worst pain). Initially, patients in the group receive information about the pelvic floor and associated symptoms, a description of the relevant anatomy and physiology of defecation, behaviour modification, and lifestyle advice.
All patients continue to use an ointment (diltiazem or isosorbide dinitrate). Anal self-massage is a treatment described to the subject by inserting the patient’s own index finger into the bladder after asking the subject to empty the bladder using appropriate “bladder emptying techniques” prior to the start of the procedure. Anal canal with lubricating cream. Patients do a “vaginal and rectal exam” to test pelvic floor muscle function. Pelvic floor muscle training (PFMT)consists of warm-up sessions that breathe freely and do not activate muscle synergies such as glutes, thighs, and abs
Group A-Ten parous women was administered for the treatment of anorectal pain. They underwent for anal self-massage to reduce the anal fissure. It is about to the use of inserting the patient’s own index finger into the anal canal with lubricant cream for 10mins twice a day for first 2 days of treatment, then the patients were instructed to perform a circular motion with the finger for 10mins twice a day for further 5 days.
Group B-Ten parous women was administered for PFMT with the help of kegel ball will be inserted into the vagina followed by three sets of 10 pelvic floor muscles contractions sustained for up to 10 seconds and two sets of three contractions sustained for up to 30 seconds a day for further 6 weeks. Participants with low muscular endurance will be instructed to hold the contraction.
Group C-Ten parous women was administered for PFMT along with Anal self-massage is used to reduce the anal fissure and it is about to the use of inserting the patient’s own index finger into the anal canal with lubricant cream for 10mins twice a day for first 2 days of treatment, then patients will be instructed to perform a circular motion with the finger for 10 minutes twice a day for further 5 days & PFMT with the help of kegel ball will be inserted into the vagina followed by three sets of 10 pelvic floor muscles contractions sustained for upto 10 seconds and two sets of three contractions sustained for upto 30 seconds a day for further 6 weeks. Participants with low muscular endurance will be instructed to hold the contraction.

Figure 2 PFMT in sitting position
Intervention for Group A with anal – self massage, Group B with PFMT and Group C with along with anal – self massage. Each group received intervention 2 days / weeks total of 6 weeks for 30 seconds. Before and after the completion of intervention, data would be obtained from the subjects.

Figure 3. PFMT in standing position
One Way ANOVA was used to find statistical difference between three groups. Paired t-test was adopted to find the statistical difference between pretest and posttest within group.
Data Analysis: The collected data were tabulated and analyzed using both descriptive and inferential statistics. All the parameters were assessed using statistical package for social science (SPSS) version 24, with a significance level of p value less than 0.05 and a 95% confidence interval set for all analysis. The Shapiro Wilk test was used to determine the normality of the data. In this study, Shapiro wilk test showed that the data was normally distributed on the dependent values of Oxford Pelvic Floor Grading Scale score (significance 0.554), Rectal Pain Scale Score (significance 0.418) & Realize Score (significance 0.454) at P > 0.05. Hence parametric test was adopted.

Figure 4. PFMT in lying position
Table – 1 Comparison of Pre & Post Oxford Pelvic Floor Grading Scale score using One Anova Test between Group A, Group B and Group C
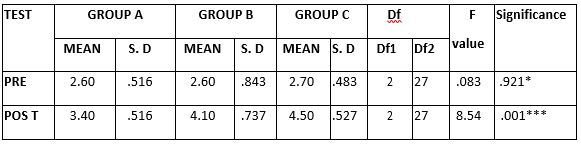
The above table reveals the Mean, Standard Deviation (S.D), ANOVA test, degree of freedom (df), F -value & P value between (Group A), (Group B) & (Group C).
This table shows that there is no significant difference in pretest values between (Group A), Group B) & (Group C) (*- P > 0.05).
This table shows that there is a significant difference in posttest values between (Group A), (Group B) & (Group C) (***- P ≤ 0.001).
Table- 2: Comparison of Pre & Post Rectal Pain Scale Score using One Anova Test between Group A, Group B and Group C.
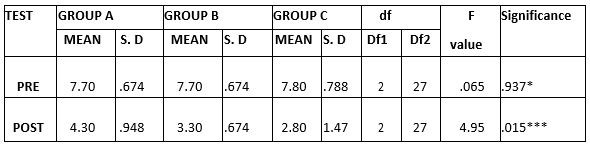
(*- P > 0.05), (***- P ≤ 0.001)
The above table reveals the Mean, Standard Deviation (S.D), ANOVA test, degree of freedom (df), F -value & P value between (Group A), (Group B) & (Group C).
This table shows that there is no significant difference in pretest values between (Group A), (Group B) & (Group C) (*- P > 0.05).
This table shows that there is a significant difference in posttest values between (Group A), (Group B) & (Group C) (***- P ≤ 0.001).
Table- 3: Comparison of Pre & Post Realize Score using One Anova Test between Group A, Group B and Group C.
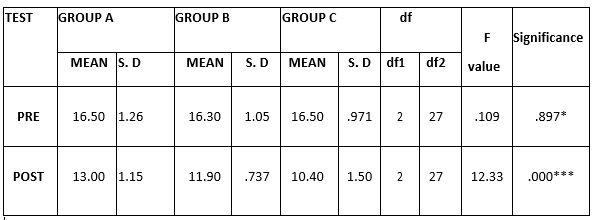
(*- P > 0.05), (***- P ≤ 0.001)
The above table reveals the Mean, Standard Deviation (S.D), ANOVA test, degree of freedom (df), F -value & P value between (Group A), (Group B) & (Group C).
This table shows that there is no significant difference in pretest values between (Group A), (Group B) & (Group C) (*- P > 0.05).
This table shows that there is a significant difference in posttest values between (Group A), (Group B) & (Group C) (***- P ≤ 0.001).
Table- 4: Comparison of Pre & Post Oxford Pelvic Floor Grading Scale Score within Group A, Group B and Group C
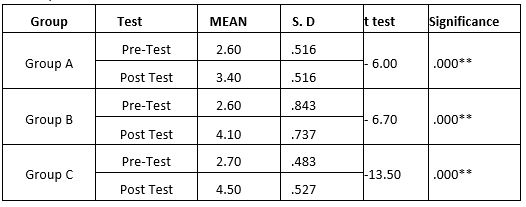
(***- P ≤ 0.001) – Significant.
The above table reveals the Mean, Standard Deviation (S.D), t test & P value within (Group A), (Group B) & (Group C).
The Table shows that a significant difference in between pretest and posttest within Group A, Group B & Group C at P ≤ 0.001.
Table- 5: Comparison of Pre & Post Rectal Pain Scale Score within Group A , Group B and Group C
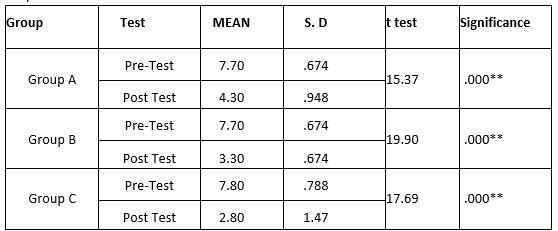
(***- P ≤ 0.001) – Significant.
The above table reveals the Mean, Standard Deviation (S.D), t test & P value within (Group A), (Group B) & (Group C).
The Table shows that a significant difference in between pretest and posttest within Group A, Group B & Group C at P ≤ 0.001.
Table -6: Comparison of Pre & Post Realize Score within Group A, Group B and Group C
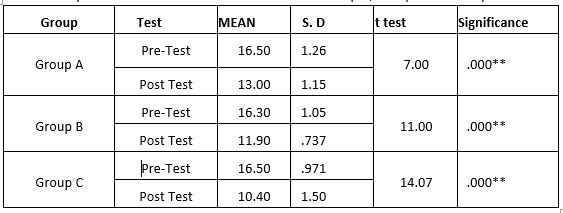
(***- P ≤ 0.001) – Significant.
The above table reveals the Mean, Standard Deviation (S.D), t test & P value within (Group A), (Group B) & (Group C).
The Table shows that a significant difference in between pretest and posttest within Group A, Group B & Group C at P ≤ 0.001.
RESULTS
On comparing mean values of Group A, Group B & Group C on Oxford Pelvic Floor Grading Scale score shows a significant increase in the post test mean values, but (Group C – Pelvic Floor Muscle Training & Self Anal Massage) shows 4.50 ± .527 which as a higher mean value is more effective than (Group B – Self Anal Massage). 4.10 ± .737 and followed by (Group A – Pelvic Floor Muscle Training) 3.40 ± .516 at P ≤
On comparing mean values of Group A, Group B & Group C on Rectal Pain Scale score shows a significant decrease in the post test mean values, but (Group C – Pelvic Floor Muscle Training & Self Anal Massage) shows 2.80 ± 1.47 which as a lower mean value is more effective than (Group B – Pelvic Floor Muscle Training) 3.30 ± .674 and followed by (Group A – Anal Self Massage) 4.30 ± .948 at P ≤ 0.001.
On comparing mean values of Group A, Group B & Group C on Realize Score shows a significant decrease in the post test mean values, but (Group C – Pelvic Floor Muscle Training & Self Anal Massage) shows 10.40 ± 1.50 which as a lower mean value is more effective than (Group B – Pelvic Floor Muscle Training) 11.90 ± .737 and followed by (Group A – Anal- Self Massage) 13.00 ± 1.15 at P ≤ 0.001.
On comparing Pretest and Post test mean values of Oxford Pelvic Floor Grading Scale score, Rectal Pain Scale score and Realize Score within Group A, Group B & Group C shows a significant difference in mean values at P ≤ 0.001.
DISCUSSION
The present study investigated the effectiveness of PFMT and Anal – self massage to enhance muscle strength among women with anorectal pain. Anorectal pain which is characterized by anal fissure, haemorrhoid, inflammatory bowel disease, proctalgia fugax and levator ani syndrome. Proctalgia fugax presents with cramping pain around the buttocks and rectum whereas, levator ani syndrome presents with dull aching or pressure like discomfort in the rectum16-19.
According to Liping Dong (2022) et., el states that the prevalence and correlates of depression and anxiety in patients with functional anorectal pain was 55% and 46% respectively and systematic review demonstrated that patients with irritable bowel syndrome have three-fold increased probability of developing either anxiety or depression, composed to healthy individuals.
The study stated that, the pelvic floor muscle training for patients with quiescent inflammatory bowel disease improved symptoms in 51 of 76 (68%) patients with evacuation difficulty and 20 of 25 (80%) patients with fecal incontinence.
This study states, anorectal pain has been described in association with a variety of organic conditions but also occurs under
A study in 2019 stated that PFMT has a therapeutic value in the patients with IBD, evacuation difficulty and fecal incontinence and also suggested that PFMT along with biofeedback has been more effective20-22.
Another study in 2021, concluded that PFMT has shown improvement in the severity of the bowel symptoms that can also lead to anorectal pain syndrome12. A study in 2021 et.al, stated that PFMT has been effective to improve pelvic floor hypertonicity14.
A study in 2013, concluded that the oxford grading scale is used as an effective measurement tool for the analysis of the pelvic floor strength among women23,24. A study in 2021, concluded that the REALISE score has an important role in the assessment and management of the severity of anal fissures25,26.
This study used the rectal pain, pelvic floor grading scale and realize questionnaire for evaluating the anorectal pain among women the other literature has also reported that the assessment tools has been effective for providing adequate outcome for the study. Our data showed that the Group C (PFMT and anal self-massage) has shown to be effective for anorectal pain when comparing to Group A (PFMT) and Group B (anal self-massage).
The results of this study showed that oxford pelvic floor grading scale, rectal pain scale and realize score showed significant difference in post-test values between Group A, B and C with a value of P<0.001.
Ethical Clearance: Ethical clearance has obtained from Faculty of Physiotherapy, Dr. MGR. Educational and Research Institute, Chennai, Tamil Nadu, Reference number: No: MPT (OBG)-06/PHYSIO/IRB/2021-2022, Dated: 29/01/ 2022.
Conflict of interest: There was no conflict of interest to conduct and publish this study.
Fund for the study: It was a self-financed study.
CONCLUSION
The present study concluded that PFMT and Anal self- massage showed effective than providing PFMT and Anal self-massage alone to women among anorectal pain. PFMT and Anal self-massage to improve muscle strength has shown improvement with a P value of <0.001 shown significant difference in men value.
Limitations of Study: The sample size was small, this study has only parous women, Age group was between 25 to 45 years only and the study duration was four weeks only.
Recommendation of the Study: Study with large sample size can be done, Study with unmarried and nulliparous women can be done.
REFERENCES
- L. Mazza E. Formento G. Fronda. Anorectal and perineal pain: new pathophysiological hypothesis. © Springer-Verlag 2004. Tech Coloproctol (2004) 8:77–83 DOI 10.1007/ s10151-004-0060-x
- Charles H. Knowles, PhD, FRCS, FACCRS (Hons), Richard C. Cohen, MD, FRCS. Cleveland Clinic Journal of Medicine Volume 89, Number 6 June 2022. Chronic anal pain: A review of causes, diagnosis, and treatment. doi:10.3949/ccjm. 89a.21102
- Sarah M. Eickmeyer, MD Anatomy and Physiology of the Pelvic Floor Phys Med Rehabil Clin NAm 28 (2017)455–460 http:// dx.doi.org/10.1016/j.pmr.2017.03.003.pm r.theclinics.com 1047-9651/17/ 2017 Elsevier.
- Strohbehn K. Normal pelvic floor anatomy. Obstet Gynecol Clin North Am 1998; 25:683–705.
- Eickmeyer SM. Anatomy and physiology of the pelvic floor. Phys Med Rehabil Clin N Am 2017; 28:455–460.
- U. Karlbom*, E. Lundin*, W. Graf * and L. Pahlman*. Anorectal physiology in relation to clinical subgroups of patients with severe constipation. 2004 Blackwell Publishing Ltd. Colorectal Disease, 6, 343–349.
- Sajad Ahmad Salati, Anal fissure-an extensive update, DOI: 10.5604/01.3001. 0014.7879, 2021, POL PRZEGL CHIR 2021: 93: 1-10 AHEAD OF PRINT, index Copernicus.
- Arnold Wald, MD. Disorders of the Anorectum 0889-8553/01. Functional anorectal and pelvic pain. Gastro-enterology clinics of North America volume 30. number 1 ,March 2001.
- J.-M. SABATE*, M. VEYRAC, F. MION, L. SIPROUDHIS§, P. DUCROTTE–, F. ZERBIB**, J.-C. GRIMAUD. Aliment Pharmacol Ther 28, 484–490. Journal compilation ª 2008 Blackwell Publishing Ltd doi:10.1111/j. 1365- 2036.2008.03759.x.
- Håvard D. Rørvik, MD, PhD a, b, d, Michael Davidsen, MSc C, Mathias Christian Gierløff, MD. Surgery Open Science. Quality of life in patients with hemorrhoidal disease. https://doi.org/10.1016/j.sopen. 2023.02.004 2589-8450/© 2023 The Authors. Published by Elsevier Inc.
- Liping Dong, Ting Sun, Ping Tong, Jia Guo & Xiaoyan Ke (2023) Prevalence and Correlates of Depression and Anxiety in Patients with Functional Anorectal Pain, Journal of Pain Research, 225-232, DOI: 10.2147/JPR.S400085. https://doi.org/10.2 147/JPR.S400085
- Hartman EE, Oort FJ, Aronson DC, Hanneman MJ, van der Zee DC, Rieu PN, Madern GC, De Langen ZJ, van Heurn LW, van Silfhout-Bezemer M, Looyaard N, Sprangers MA. Critical factors affecting quality of life of adult patients with anorectal malformations or Hirschsprung’s disease. Am J Gastroenterol. 2004 May;99(5):907-13. doi: 10.1111/j.1572-0241.2004.04149. x. PMID: 15128359.
- Dani¨elle A. van Reijn-Baggen a,b,* , Henk W. Elzevier b , Rob C.M. Pelger b , Ingrid J. M. Han-Geurts. Pelvic floor physical therapy in the treatment of chronic anal fissure (PAF-study): Study protocol for a randomized controlled trial. 2451- 8654/© 2021 The Authors. Published by Elsevier Inc. Contents lists available at ScienceDirect Contemporary Clinical Trials Communic- ations journal homepage: www. Elsevier .com/locate/conctc. https://doi.org/10.10 16/j.conctc.2021.100874.
- Daniëlle A. van Reijn-Baggen1,3 · Henk W. Elzevier2 · H. Putter4 · Rob C. M. Pelger3 · Ingrid J. M. Han-Geurts. Techniques in Coloproctology (2022). Pelvic foor physical therapy in patients with chronic anal fssure: a randomized controlled trial 26:571–582, https://doi.org/10.1007/ s101 51-022-0261b8-9.
- Danielle A. van Reijn-Baggen, MSc,1,2 Ingrid J.M. Han-Geurts, MD, PhD,1 Petra J. Voorham-van der Zalm, PhD,2. Sex Med Rev 2021;000:1−22. Pelvic Floor Physical Therapy for Pelvic Floor Hypertonicity: A Systematic Review of Treatment Efficacy. https://doi.org/10.1016/j.sxmr.2021.03.002.
- Liping Dong, Ting Sun, Ping Tong, Jia Guo & Xiaoyan Ke (2023) Prevalence and Correlates of Depression and Anxiety in Patients with Functional Anorectal Pain, Journal of Pain Research, 225-232, DOI: 10.2147/JPR.S400085 To link to this article: https://doi.org/10.2147/JPR.S40.
- Direnc Yigit, Mehmet Ilker Turan, Nedim Akgul. A rare cause of acute anal pain: strangulated hemorrhoids in a perianal fistula. Ann Ital Chir, 2022; 11 – July 5 pii: S2239253X22037069 Online Epub.
- Fabio Gaja, Ivano Bivianob, Laura Candelo rob, Jacopo Andreuccetti. Annals of Gastroenterology (2017) 30, 1-4. Anal self-massage in the treatment of acute anal fissure: a randomized prospective study. DOI: https://doi.org/10.20524/aog.2017. 0154. 2017 Hellenic Society of Gastroenterology.
- Da Roza T, Mascarenhas T, Araujo M, Trindade V, Jorge RN. Oxford Grading Scale vs manometer for assessment of pelvic floor strength in nulliparous sports students. Physiotherapy.2013Sep;99(3): 207-11.doi: 10.1016/ j. physio. 2012. 05.014. Epub 2012 Oct 15. PMID: 23219628.
- Picciariello1,3 · P. Lobascio1 · L. Spazzafumo2 · M. Rinaldi1 · R. Dibra1 G. Trigiante1 · R. Laforgia1 · A. Pezzolla1 · D. F. Altomare. Techniques in Coloproctology https://doi.org/10.1007/s10151-021-0245 9-y. The REALISE score: a new statistically validated scoring system to assess the severity of anal fissures. May 13 2021.
- Annette C. Dobben Maaike P. Terra Bary Berghmans Marije Deutekom. Functional changes after physiotherapy in fecal incontinence. Int J Colorectal Dis (2006) 21: 515–521 DOI 10.1007/s00384-005-0049-6. # Springer-Verlag 2005.
- Fuentes-Aparicio, L.; Arranz-Martín, B.; Navarro-Brazález, B.; Bailón-Cerezo, J.; Sánchez-Sánchez, B.; Torres-Lacomba, M. Postural Sensorimotor Control on Anorectal Pressures and Pelvic Floor Muscle Tone and Strength: Effects of a Single 5P® LOGSURF Session. A Cross-Sectional Preliminary Study. Int. J. Environ. Res. Public Health 2021, 18, 3708. https://doi.org/ 10.3390/ijerph18073708.
- Esther Bols,1,2* Bary Berghmans,3 Rob de Bie,1,2, Rectal Balloon Training as Add-On Therapy to Pelvic Floor Muscle Training in Adults with Fecal Incontinence: A Randomized Controlled Trial, DOI 10.1002/nau.21218, August 2011.
- E. A. Walker’, A. N. Gelfand’, M. D. Gelfand2, C. Green’ and WJ Katon’. Chronic pelvic pain and gynecological symptoms in women with irritable bowel syndrome.J. Psychosom. Obstet. Gynecol. 17 (1996) 39-46.
- E. A. Walker’, A. N. Gelfand’, Chronic pelvic pain and gynecological symptoms in women with irritable bowel syndrome, J. Psychosom. Obstet. Gynecol. 17 (1996) 39-46.
- Angela J Khera, Janet W Chase, * Michael Salzberg, * Systematic review: Pelvic floor muscle training for functional bowel symptoms in inflammatory bowel disease, March 2019, doi:10.1002/jgh3.12207.
- Dong L, Sun T, Tong P, Guo J, Ke X. Prevalence and Correlates of Depression and Anxiety in Patients with Functional Anorectal Pain. J Pain Res. 2023 Jan 26; 16:225-232. doi: 10.2147/JPR.S400085. PMID: 36726856; PMCID: PMC9885881.
| Citation: Deepthi RNV, Daranisri. J, Jibi Paul (2024). Pelvic Floor Muscle Training and Anal Self-Massage to Enhance Muscle Strength and Quality of Life in Women with Anorectal Pain, ijmaes; 10(1); 1779-1790 |

Leave a Reply