Soong Shui Fun1, Hamidah Hassan2, *Mazlinda Musa3, Chyretta Burno4, Mohd Ishkandar Nazlan5, Wihelmina Michael6
Authors:
1-6Department of Nursing, Faculty of Medicine and Health Sciences, Universiti Malaysia Sabah, Kota Kinabalu, Sabah, Malaysia
Corresponding Authors:
*Department of Nursing, Faculty of Medicine and Health Sciences, Universiti Malaysia Sabah, Kota Kinabalu, Sabah, Malaysia, Email id: mazlinda@ums.edu.my
Abstract
| Introduction: The Ministry of Health Malaysia over the last 20 years has initiated healthy lifestyle campaign to curb obesity but the issue has remained an escalating problem affecting Malaysians. Obesity among students in higher institute is a concern. Undergraduate student nurses as role-model advocating health, being overweight can be a problem. This study is to identify BMI status and determine associated lifestyle factors among undergraduate nurses in UMS. Methods: The study deployed a cross-sectional descriptive survey using a questionnaire to empirically asses BMI status and associated dietary and exercise practice among student nurses. Ethical clearance for the study was obtained from University Malaysia Sabah (UMS) Research Ethical Committee (REC) and as well as respondents` consent. A total of 100(N) nursing students were selected through stratified sampling by year of study Random sampling for each year of study was done using full name list generated using Microsoft excel. The study tool consists of a validated instrument which captured the respondent’s demographics, BMI index, Healthy Eating Practice Index, and Exercise Practice Inventory. Results: Among the 100 student nurses in this study, 28 students had BMI index of more than 24.9 (either being overweight, obesity Type I or Type II). Students from final Year 3 are significantly overweight (p=0.03) compared to Year 1 or Year 2 students. Comparing respondents with optimum BMI and non-optimum BMI, students who are overweight had significantly poorer healthy eating practice scores and poorer exercise practice scores. Conclusion: Findings from this study revealed that 1 in 4 nursing students are overweight mostly related to poor lifestyle habits. These findings raise the rhetoric and implication of overweight nurses as health care role –models. Keywords: Body Mass Index, Student Nurses, Eating Practice, Exercise Practice, Role-model Received on 30th April 2021, Revised on May 15th 2021, Accepted on 25th May 2021. DOI:10.36678/IJMAES.2021.V07I02.004 |
INTRODUCTION
Obesity and overweight have both been described as anomalous accumulation of excessive body fat which may be harmful to health. Increased mortality and substantial morbidity are associated with obesity due to its impact on type 2 diabetes, cardiovascular (Cercato and Fonseca, 2019) 4, gastro-intestinal (Su, 2017)22, Osteoarticular (Natale et al, 2003)14 and reproductive disease (Crujeiras and Casanuera, 2014)5 and certain cancers. It is the single most important risk factor for type 2 diabetes. Obesity and its consequences represent a major unmet need for improved therapies and prevention strategies.
Body mass index (BMI) is explained as a value derived from the mass and height of a person. The World Health Organization (WHO) criteria for obesity based on the BMI guidelines is BMI equals weight in kilograms divided by height in meters squared (BMI = kg/m 2) Using BMI, it is possible to classify the degree of obesity by reference to internationally accepted ranges, starting from underweight (BMI & lt;18.5 kg/m 2), normal (BMI 18.5–24.9 kg/m 2), overweight (BMI 25.0–29.9 kg/m 2) and obese (BMI ≥ 30 kg/m 2)1,11 .
Body mass index is also understood as a number that reflects body weight adjusted for height. It indicates a person’s the body fatness that may lead to health problems. Normal accepted values are as follows: underweight 18.5, normal weight is 18.5-25. Values of 25-29.9 are considered overweight and values of 30 or higher are considered obese (Pasco et al, 2014)17.
According to (Prentice 2005)16 who stated WHO those resource poor countries would be threatened with a double burden disease of obesity and accompanying non-communicable disease. WHO warned that future burden of obesity and diabetes will affect developing countries with a likely increase of diabetes within the next 2 decades. Obesity not only affects rich countries such as US and Europe but can find its way into urban areas through mechanized agriculture with big companies providing cheap oily foods and carbohydrates. Workers have much labour saving mechanized devices and affordable transportation which enable them to lead a sedentary life and past times like watching television. In another study, Hossian et al (2005)18 stated the growing prevalence of overweight and obesity is causing an enormous increase of diabetes and hypertension cases.
Today, more than 1.1 billion adults worldwide are overweight, and 312 million of them are obese. Philip and James (2004)19 In their studies found that prevalence of obesity in Western and Westernizing countries such as the United States, England, Brazil, and Japan, have a progressive increase in obesity rates. There is a relationship seen between education level/socioeconomic status and obesity prevalence. Hence, obesity is increasingly seen as a feature of the poor. Rampal et al (2007)21 reported that in Malaysia, rapid economic development enhanced increased urbanization, affluence, lifestyles changes and nutritional status of the population.
This influences the diet of people. Urban dwellers with dual working spouses tend to eat out in restaurants and fast food outlets or stalls. This indicates that obesity prevalence in 2004 was 280% higher than that in 1996. At this level, the obesity prevalence in Malaysia is higher than that in France (7%) and United Kingdom (9%) but lower than that in the United States (20.9%), Sidik (2007)24 also agreed that there is rapid and marked socioeconomic advancement in Malaysia in the past 2 decades has brought about significant changes in the communities and their life styles. He found that there are significant changes in the dietary patterns of Malaysians where more families eat out, busy executives skip meals, and the younger generations miss breakfast, relying a lot on fast food. The women tends to be more obese than their male counterparts as they manage the food at home with frequent opportunities to consume food, more likely to have greater volumes of food available as well as buying home food from restaurants, food-stalls and fast-food centers for their families as they are working mothers. Hence many Malaysians are at risk of being overweight or obese.
According to Ministry of Health Malaysia, the obesity statistics showed prevalence in adults increased from 17.7 per cent (or 3.3 million people) in 2015 to 19.7 per cent in 2019. There was a slight increase in overweight from 30 per cent in 2015 to 30.4 per cent in 2019. This means half of Malaysian adults (50.1per cent) were overweight or obese as of 2019 (MOH, 2019)13.
According to a systematic analysis of global data on the prevalence of overweight and obesity in adults, the prevalence of obesity in Malaysia, reported 11.4% in males; 16.7% in females was observed to be lower than that reported in Western countries, such as Australia (27.5% in males; 29.8% in females) This shows that Malaysian females are more obese than the males Diet-related chronic diseases, including obesity are increasing in affluent urban populations and obesity is significantly higher among women as compared to men. With the above gaps and problems, this study aims to survey body mass index, determine eating habits and exercise practice among UMS nursing students. Obesity has remained an issue affecting Malaysians even though Ministry of health has over the over the last 20 years initiated healthy life campaign programs to reduce and halt obesity without much efficacy.
According to Yahia et al (2008)26, obesity among students in higher learning institute has also become increasingly prevalent and become an issue of concern. Consensus from literature attests that obesity in young adults will have serious consequences in later life with high risk of developing lifestyle diseases such as diabetes and hypertension (Pulgaron et al, 2014)20. As of date, there had been no specific study done in UMS to examine the prevalence of obesity among medical and nursing students and thus the justification for this study. Findings from this study can help identify the prevalence of obesity among the students so that effective strategies can be implemented to address the issue.
METHODOLOGY
This study deployed a cross-sectional descriptive survey using a questionnaire to empirically assess BMI status and associated dietary and exercise practice. This cross sectional survey collects information from a sample drawn from a population at one point of time. We used a survey to collect quick, inexpensive and accurate information from a large group of people. It is used to explain relationships and differences between variables. This study was conducted in University Malaysia Sabah among nursing students for duration of 6 months, started from September 2019 to February 2020.
The study sample of 100 respondents were from year 1, year 2 and year 3 nursing students (year 1 = 35, year 2 =35, and year 3 =30). The respondents were selected through stratified sampling by year of study. Randomization for each year study was done using full name list generated by Microsoft excels. The inclusion criteria include respondents who were willing to participate and consented for this study. They are UMS nursing students from year 1 until year 3. Exclusion criteria disqualify nursing students who were unwilling to participate in the study The Statistical data from this study is used to gather, review, analyze and draw conclusions so that recommendations can be studied to improve the current issue a standardized structured questionnaire was used. The questionnaire consists of a validated instrument adapted from a previous study to capture respondent’s data. The questionnaire consists of 2 parts. Part A Consisted of questions on demographic variables (age, race, gender,) and BMI index. Part B consists of questions related to body mass index, healthy eating practice index and exercise practice inventory.
Respondents are given a brief description of the study and how to answer the questionnaire. The questionnaire was distributed to respondents by using Google form and checked by researcher. Returned questionnaires will be checked for completeness. Collected data from the questionnaire was analyzed using SPSS software and descriptive statistics. The findings were presented in mean, mode and frequency.
RESULTS
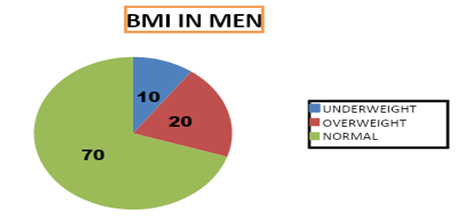
The graph shown that 70% of male nursing student is in range of normal weight, 10% of them are underweight and 20% of them are overweight.
The graph shows that 66.25% of female nursing student is in range of normal weight, 16.25% of them is underweight and 17.5% of them is overweight The above result showed that male nursing student have higher percentage in normal weight compare to female nursing student. There are not much differences of percentage in context of overweight BMI. The difference of the percentage is just 2.5%.
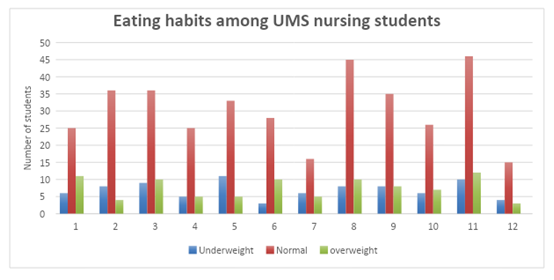
Eating habits among UMS nursing students Underweight Normal overweight Based on the table above, it shows a graph of the total BMI status with the student eating habits7.
1) I take sweet drinks almost daily. For the first question, for underweight there is only 6/14 students (42.9%) that take sweet drinks, while normal weight is 25/61 students (40.9%). For the overweight there is 10/15 students (73.3%). These shows that overweight students are the highest percentage while the normal weight students are the lowest percentage that taking sweet drinks daily.
2) I like to eat Titbit during study, while watching TV or online. For the second question, for underweight students there are 9/14 (64.2%) like to eat Titbit. For the normal weight students were 36/61 (59%), while the overweight students are 10/15 (66.6%). These shows that overweight students are the highest percentage while the normal weight students are the lowest percentage that like to eat Titbit during study, while watching TV or online.
3) After lunch or dinner, I still feel hungry. For the third question, for underweight students there is 11/14 (78.5%) that still fell hungry even after taking lunch or dinner. 33/61 students (54%) for normal weight, while 5/15 students (33%) for overweight. These shows that underweight students are the highest percentage while underweight students are the lowest percentage that will still hungry.
4) I often eat during midnight (supper). For the fourth question, according to the graft, 6/14 underweight students, (42.8%) often eat during midnight. 16/61 students (26.2%) for normal weight, while 5/15 students (33%) for overweight. The highest percentage that often eats during midnight is underweight, while the lowest percentage is normal weight.
5) If there is free food, I will eat as much as possible. For the fifth question, for underweight there are 8/14 students (57.1%). While for normal weight is 35/61 students (57.4%), and for overweight there is 8/15 students (53.3%). This shows the highest percentage is normal weight students and the lowest percentage is overweight students.
6) I prefer fried chicken rather than steamed chicken8. For the sixth question, for underweight there is 10/14 students (71.4%), while for normal weight is 46/61 students (75.4%), and for the overweight is 12/15 students (80%). The highest percentage is overweight while the lowest percentage is underweight.
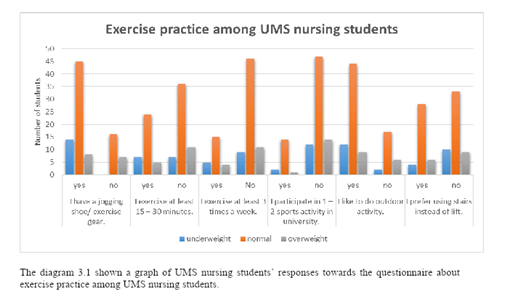
Figure 2, Exercise practice among UMS nursing students. The Figure 3, showed a graph of UMS nursing students’ responses towards the questionnaire about exercise practice among UMS nursing students.
1) I have a pair of jogging shoes/ exercise gear. For the first question, all the 14 underweight students, about half of the overweight students which is 8/15 (53%) and majority of students with normal weight which is 45/61 (74%) have their jogging shoe/exercise gear. These shows that underweight students have the highest percentage and overweight students have the lowest percentage of having a jogging shoe/exercise gear.
2) I exercise at least 15-30 minutes9. For the next question, half of the underweight students which is 7/14 (50%) students exercise at least 15-30 minutes. There are fewer overweight students and normal weight students which are 5/15 (33%); 24/61 (39.3%) exercise at least 15-30 minutes.
3) I exercise at least 3 times a week. The next question result shows there are fewer students that exercise at least 3 times a week for all students’ categories. Only 5/14 (36%) of underweight students, 4/15 (27%) of overweight students, and 15/61 (25%) of student with normal weight exercise at least 3 times a week.
4) I participate in 1-2 sports activity in the university. For the fourth question, most of the students from all categories didn’t participate in 1=2 sports activity in their university. 14/61 (23%) of the students with normal weight, only 2/14 (14%) of underweight students, and 1/15 (7%) of overweight student were participated in 1-2 sports activity in their University.
5) I like to do outdoor activity. Result for the fifth question shows that most of the underweight students which is 12/14 (86%) like to do outdoor activity. More than half of students with normal weight and overweight like to do outdoor activity. 44/61 (72%) students for normal weight, and 9/15 (60%) students for overweight.
6) I prefer using the stairs instead of lift. Result for the last question shows, almost half of the students with normal weight, which is 28/61 (46%) students, 29% of underweight students which is 4/14 students, and 40% of the overweight students which is 6/15 students prefer to use stairs instead of lift. The rest of them prefer using lift instead of stairs.
DISCUSSION
According to the Harvard T.H. Chan, School of Public Health, a person tends to take more calories at the end of the day if she consumes a large amount of sugary drinks during the day. However, when a person consumes solid food, she tends to take fewer calories at a later meal time to compensate for a large meal eaten earlier.
This compensatory effect is not present after consuming soft drinks. Therefore, people who drank sugary drinks were more likely to be obese than those who did not. Based on the research questionnaire, overweight students have the highest percentage that takes sweet drinks almost daily. This shows that taking sweet drinks can influence the student’s weight.
According to Bastami, Alavijeh, Mostafavi (2019)2, University students tend to make their own food choices. They lack knowledge of healthy food choices that may affect eating habits and nutritional status negatively. University students had frequent snacking habits and had a higher frequency of fast food consumption. Eating titbits during study while watching TV or online can affect their BMI status.
Berry (2019)3 stated in the newsletter Medical news today that people who is dieting may feel hungry most of the time. Consuming fewer calories than the body requirement can cause the body to produce a hormone called ghrelin which is released in the stomach. A low-calorie diet can increase ghrelin production and cause hunger, even after a person has just eaten. (Berry, 2019)3 said eating at night has long been associated with weight gain. Spencer (2017) 25 used nutritionist Adele Davis slogan “eat breakfast like a king, lunch like a prince and dinner like a pauper.”
However, our current rational wisdom is based on the fact that that a calorie is a calorie, regardless of when it is eaten. The causes for weight gain are simply eating more calories than is needed. Nutrition experts call this the calorie in/calorie out theory of weight control. Spencer (2017) 25 has stated as agrees that a person can eat anytime during the day or night.
The important thing is to know how much food is eaten and how much physical activity is done. This balance will determine whether a person will gain, lose, or maintain her body weight. Spencer (2017) 25 believes that eating at night does not affect the body weight.
According to Mc Donell (2017)12, many people enjoy fried foods. Which are high in calories and trans- fat, thus can have negative effects on health. Fried foods contain more calories than other methods of cooking food. Consuming big quantity of fried food will have a significant increase in calories
Hockey et al (2014) 10 stated that it is important to have the right equipment before committing to start an exercise program. The person should have a pair of athletic shoes as this provides comfort and safety to the wearer. Based on the research questionnaire result, overweight students have the least percentage of having a shoe/exercise gear. This shows that only a few of overweight nursing students have the effort to keep their body fit. (Questionnaire; I have a pair of jogging shoes/exercise gear) Referring to the result, the lowest percentage of students that exercise at least 15-30 minutes also held by the overweight students’ category which is only 33% of them.
According to Nikkola (2011)15 exercises plays a critical role in long-term weight management, and committing to only 15 minutes per day is not likely enough to support weight loss or management. This shows clearly that UMS nursing students those exercise less than 15 minutes per day is one of the factors of overweight BMI status. Nikkola, (2011)15 and Friedrich (2018)8, personal trainer, a conditioning coach, and sports therapist wrote an article about optimal amount of exercise per week and how to reduce weight effectively. According to him, “Beginners, as well as more advanced athletes, will see the biggest benefits if they work out three to four times a week”. This exercise practice was not practiced by majority of UMS nursing students.
By referring to an article written by (Diranian 2017)6 quote “To lose weight and stay in shape, it is important to burn more calories than you consume. Exercise and sports can burn significant calories. The number of calories you burn depends on your weight and physical capabilities, the sport or activity and intensity level.” However, most of UMS nursing students did not participate in 1-2 sports activity.
Outdoors offer several inexpensive and free activities to stay fit and help lose weight. Since more than half of overweight students like to do outdoor activity, this factor is not one of the main factors of obesity among UMS nursing students.
Smith (2008)23 quoted “Increasing the number of stairs climbed in a day improves fitness and reduces body fat. However, using the lift instead of stairs is not affecting much in BMI status of UMS nursing students.
Ethical clearance: Ethical clearance was obtained from the ethic committee Faculty of Medicine & Health Sciences, University Malaysia Sabah (UMS), reference no is JKE tika 3/19 (10) and informed consent from the respondents.
Conflicts of Interest: There is no conflict of interest in this study.
Fund for the study: This is self-funded study.
CONCLUSION
The results of this study found that socio-demographic factors such as gender and ethnicity were significantly associated with obesity among male and female nursing in this study. UMS nursing students should be concern about their body mass index to avoid obesity by taking a healthy diet and practice appropriate exercise. They are supposedly role models advocating health and being overweight can be an image problem.
The findings of this study can provide baseline data for monitoring the effectiveness of eating habits and exercise for the control of obesity in nursing students in UMS. Resources for the prevention and control of obesity can be mobilized and allocated based on the factors identified to be associated with obesity.
Further studies need to be done to assess the main contributing factors associated with obesity in this group of students. The respondents are busy all the time probably because this study was conducted during clinical posting week. It was difficult to approach the nursing students to distribute the questionnaires and asked their consent to answer the questionnaires as everyone was in different shift and different hospital posting. In addition, they were busy doing their own assignment. For ourselves, we experienced difficulties in seeing and meeting up with each other because we were in clinical posting and was posted into different wards and on different shift duty.
Future prospective in future, we should involve other nursing students from different colleges in our study. We can use Google Form to share our questionnaires. Through this way, we can distribute the questionnaires faster and get more respondents.
We should distribute the questionnaires to the respondents on weekends as we do not have clinical posting during that time and they are not too busy. They might have time to fill up the questionnaires sincerely.
REFERENCES
- Andrew, M. (2006). The emerging epidemic of obesity in developing countries. International Journal of Epidemiology. Vol 35, Issue 1, Pages 93–99. https:// doi.org/10.1093/ije/ dyi272
- Bastami, F., Alavijeh, F.Z., (2019). Mostafavi, F. Factors behind healthy snack consumption at school among high-school students: a qualitative study. BMC Public Health. ; Volume 19; Article number: 1342.
- Berry, J. (2019). 17 Reasons for always feeling hungry. Medical news today: newsletter. February 22; https://www. medicalnewstoday.com/articles/324523.
- Cercato. C., (2019). Fonseca, F. A. Cardiovascular risk and obesity. BMC: part of Springer. Diabeto- logy & Metabolic Syndrome. Volume11; number: 74.
- Crujeiras, A.B., Casanuera, F. F. (2015). Obesity and the reproductive system disorder: epigenetic as a potential bridge.Human Reproduction Update, Volume 21, Issue 2, March/April, Pages 249–261. Retrieved August 23, 2020; https://academic.oup.com/humupd/article
- Diranian,S. (2017).What Sport Burns the Most Calories Per Hour. LiveStrong.com;Retrieved September 24, 2020;https://www.livestrong.com/article/474836.
- Elmagd, M.A. (2016). Benefits, needs and importance of daily exercise International Journal of Physical Education. Sports and Health 2016; 3(5): 22-27; https://www.researchgate.net/ publication /306118434.
- Friedrich, S. (2018). How Often Should You Exercise per Week to Lose Weight: Runtastic. Retrieved September 24, 2020; https://www.runtastic.com/blog/en.
- Harvard T.H. Chan (2019). School of Public Health (n.d). The nutrition source. Retrieved August 27, 2020;https:// www.hsph.harvard.edu/nutritionsource/healthydrinks/sugarydrinks.
- Hockey,J., Dilley , R., Robinson,V. (2014). There’s not just trainers or non-trainers, there’s like degrees of trainers’: Commoditisation, singularisation and identity. Journal of material culture. October 3, 2020; doi/10.1177 /1359 183514560665.
- Kerr, M. Exercise and weight loss: Health line. (2017). Retrieved September 24, 2020 from https://www.healthline.com/health/ exercise- and-weight-loss.
- Mcb Donell, K. (2017). Why is fried food bad for you? Health line. August 20, 2020; https://www.healthline.com/nutrition/why-fried-foods-are-bad.
- Ministry of Health Malaysia, (2019). Malaysia obesity statistics; https://www. google.com/ search? ei=HjZ0X5nnLriO4.
- Natale, S., Tiraferri, F ., Tartaglia, A., Moscatiello, S ., Marchesini Reggiani ,L ., Villanova N., Forlani, G., Melchionda, N., Marchesini, G. (2003). The burden of obesity on everyday life: a role for osteoarticular and respiratory diseases. Europe PMC. Retrieved August 24, 2020 from https://europepmc.org/article/med/ 15000439.
- Nikkola,T. (2011). Exercise is more than calories out: Lifetime weight loss. Retrieved September 27, 2020 from http:// www. lifetimeweightloss.com/blog/2011/2/2/20.
- Prentice, R.L. (2005). Cohort Study. In Encyclopedia of Biostatistics (eds P. Armitage and T. Colton). https://doi.org/10.1002/ 0470011815.b2a03032.
- Pasco,J. A., Holloway, K.L.,Dobbins, A.G., Kotowicz , M.A.,Williams ,L.J.,Brennan S.L. (2014). Body mass index and measures of body fat for defining obesity and underweight: a cross- sectional, population-based study. BMC: Part of Springer nature. Retrieved August 23, 2020; https://bmcobes.biomedcentral. com/ articles/10.1186/2052-9538-1-9.
- Hossain,P., Kawar, B., Nahas, M.E.(2005). Obesity and Diabetes in the Developing World-A Growing Challenge. The new England Medical Journal. Retrieved September 28, 2020; https://www. nejm.org/ doi/full/10.1056/nejmp068177.
- Philip, T. James, C.B.E.,(2004).Obesity: The worldwide epidemic. Journal Clinics in dermat- ology. Volume 22 issue August 2004.page 276-280. Retrieved September 28, 2020 from https://doi.org/ 10.1016/j.clindermatol.2004.01.010.
- Pulgaron, E. R., Delamater, A, M. (2014). Obesity and Type 2 Diabetes in Children: Epide- miology and Treatment. Retrieved August 24, 2020; https:// www. ncbi.nlm.nih.gov/ pmc/ articles/ PMC 4099943.
- Rampal, L., Rampal,S., Khor,G.L., Azhar, M.Z.,Shafie, O., Ramlee, R., Sirajoon, N.A.G., Jayanthi,K.(2007). A national study on the prevalence of obesity among 16,127 Malaysians. Retrieved September 29, 2020 from http://apjcn.nhri.org.tw/ server/ APJCN/ 16/3/561.
- Su, Y.N. (2017). Obesity-Related Digestive Diseases and Their Pathophysiology. PMC Gut liver.Retrieved August23,2020; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5417- 774.
- Smith, R. (2008). Walking upstairs rather than standing in lift reduces risk of early death. Thetelegraph. Retrieved September 25, 2020 from https://www.telegraph. co.uk/ news/ worldnews/2656456.
- Sidik, S.M., Rampal, L. (2009). The prevalence and factors associated with obesity among adult women in Selangor. Malaysia. Asia Pacific Family Medicine volume 8, Article number: 2. Retrieved September 28, 2020 from https://link. springer.com/ article/10.1186/ 1447-056X-8-2.
- Spencer, C. (2017). Breakfast: The most important meal of the day? International Journal of Gastronomy and Food Science. Retrieved August 22, @ 020 from https://www. sciencedirect.com /science/ article/ pii/S1878450X17300045.
- Yahia, N., Achkar, A., Abdallah, A., Rizk , S. (2008). Eating habits and obesity among Lebanese University students, Nutrition Journal volume 7, Article number: 32. Retrieved August 23, 2020 from https://link.springer.com/article/10.1186/1475- 2891-7-32
| Citation: Soong Shui Fun, Hamidah Hassan, Mazlinda Musa, et. al. Body Mass Index status and associated lifestyle factors among Nursing students in University Malaysia Sabah. ijmaes; June 2021; 7 (2); 1003-1012. |

Leave a Reply