Jomi John1, Jince Augustine2
Author:
1Jomi John, MPT Musculoskeletal and Sports-student, CPAS School of Medical Education, Gandhinagar, Kottayam, Kerala, India, Mail id: jomijohn333@gmail.com
Co Author:
2Associate Professor of Physiotherapy, CPAS School of Medical Education, Gandhinagar, Kottayam, Kerala, India
ABSTRACT
Background and objectives: Plantar fasciitis is a commonly confronted orthopedic problem due to inflammation of the plantar fascia and the perifascial structures. The literature attributes plantar fasciitis is due to pathologic biomechanics such as excessive pronation, high arched foot, windlass mechanism and low back disabilities. Current evidences suggest that faulty biomechanics that lead to plantar fasciitis may be started from gluteal muscles weakness. The purpose of the study is to find out the effectiveness of gluteal muscles strengthening exercises to reduce pain and improve lower limb function in patients with plantar fasciitis.
Methods: 30 subjects those satisfying the inclusion criteria were recruited for the study. Subjects were then allocated to two groups- Group A (control group) and Group B (experimental group), 15 in each group. Subjects in group A received conventional treatment and subjects in group B received experimental treatment of gluteal muscle strengthening exercises with conventional stretching exercise. Pain was measured using Numeric Pain Rating Scale (NPRS) and lower limb functions was measured using Star Excursion Balance Test (SEBT).
Results: The post test score of SEBT and NPRS of control and experimental group were analysed using two sample t test and paired t test. The data analysis showed statistically significance difference in the post test scores of SEBT and NPRS of experimental group over control group at 5% level.
Conclusion: This study concluded that gluteal muscles strengthening exercises helps in improving lower limb function and reduction in pain in patients with plantar fasciitis.
Keywords: Plantar fasciitis, Gluteal muscles, Star Excursion Balance Test, Numeric Pain Rating Scale
| Received on 8th May 2020, Revised on 22nd May 2020, Accepted on 29th May 2020 |
DOI:10.36678/ijmaes.2020.v06i02.003
INTRODUCTION
Plantar fasciitis is a commonly confronted orthopaedic problem treated by healthcare professionals. It is generally known as plantar heel pain. It is an inflammatory condition of plantar fascia and perifascial structures at its anatomical insertion site on the calcaneus. It is often an overuse syndrome which causes impairment of activity and results in disability 1- 6.
The epidemiological studies shows that approximately one million patients visits per year are due to plantar fasciitis, though the exact incidence and prevalence of plantar fasciitis remains unknown. It is thought to occur in 83 percent active working adults between the age of 25 and 65 years out of the 10 percent of victim’s worldwide.7
There is a body of literature on the association of plantar fasciitis with advancing age. Degenerative changes may cause decrease in shock absorption due to reduction in elasticity and then makes plantar fascia more prone to injury. There is no significant variation in prevalence between women and men. Obese individuals are 14 times more prone for developing chronic plantar fasciitis 8-12.
The diagnosis of plantar fasciitis is based on the clinical manifestations (eg. Pain on initial step after rest) and tenderness on the calcaneal insertion of the plantar fascia.7 Individuals with PF frequently wait for several months after the onset of symptoms before they seek medical care, then it affects the prognosis of conservative care badly. In addition 18-50 percent of individuals will still show a temporary improvement with symptoms recurrence eventually13-16.
The results of various studies suggest that faulty biomechanics of lower limb musculature could be involved in PF etiology. Gluteus maximus are the key muscles of hip extension and support lateral rotation, abduction and adduction. Gluteus medius and gluteus minimus play the role of primary abductors of hip17.
There is a decrease in the strength of hip extension and lateral rotation due to weak gluteus maximus. The hamstrings muscle can work in compensation to weak hip extensors and this leads to tightness of hamstrings, thus causing an increase in knee flexion, which in turn cause prolonged forefoot loading and encourages the windlass mechanism2,18,19.
The windlass mechanism is a principle that ensures a thorough basis for the biomechanical factors and stresses that cause plantar fascia injury. Windlass is the winding of a rope or cable. Likewise the winding of plantar fascia reduces the distance between the calcaneus and metatarsal which raises the medial longitudinal arch3,19.
Some studies conclude plantar fasciitis as a resultant of faulty biomechanics such as excessive pronation.A reduction in the strength of the hip abductors and lateral rotators disturbs the dynamic alignment and can cause adduction and medial rotation of the hip and dynamic knee valgus which is directly involved with pronation of foot 3,20,21.
The treatment techniques for PF include passive joint manipulation of the ankle and foot; myofascial manuevers of the gastrocnemius, soleus muscles, and plantar fascia; neural mobilization of the tibial nerve; and stretching of plantar fascia and triceps surae; strengthening of hip abductors and external rotators. Electrotherapy modalities like cryotherapy, ultrasound, laser and kinesio taping are found to be effective in reducing plantar heel pain22,23.
The purpose of this study is to find out the effectiveness of gluteal muscles strengthening to reduce pain and functional disability in patients with PF.
Objectives of the Study: To find out the effectiveness of Gluteal muscles strengthening exercises to reduce pain in patients with plantar fasciitis. And also to find out the effectiveness of gluteal muscles strengthening exercises on lower limb function in patients with plantar fasciitis.
METHODOLOGY
This Study was conducted atDepartment Of Physiotherapy, SH Medical Centre, Kottayam. Total 30 samples were selected for this study.This was an experimental study and the samples were divided into two groups by purposive sampling method. The study conducted for duration of 10 months.
Inclusion criteria: Subjects withNormal limb length, Both males and females, Pain upon palpation on the plantar face of the heel, Insidious onset of pain, Pain that accentuates after long periods of upright activities or after rest and Reduction in pain following light activities were included for this study.
Exclusion criteria: Pain medication, History of lower limb surgery, History of lower limb fracture, Neurological disease, Achilles tendinopathy, Meta-tarsalgia, acute ankle sprain, Tarsal tunnel syndrome, BMI higher than 35 kg/m2 were excluded from the study.
Procedure: Thirty subjects who fulfil the inclusion criteria will be selected and divided into two groups. Group A and group B with fifteen patients in each group. Group A (control group) undergoes conventional therapy which include four daily stretching exercises with 2 sessions/week for a period of eight weeks (three 30-s sets).
Stretching of hamstring and ankle plantar flexors (straight leg raise in the supine position), Self-stretching of the calf muscles. The patient leaned forward in the standing position with the affected foot farther away from the wall, while keeping the heel on the floor; the soleus muscle was emphasized with the knee flexed and the gastrocnemius muscle with the knee extended. Self stretching of the plantar fascia: in the sitting position, the patient crossed the affected foot over the contra lateral thigh and performed passive extension of the metatarso-phalangeal joints will be given for this group.
Group B (experimental group) undergoes conventional therapy with Gluteal muscles strengthening:
For Gluteus medius and gluteus minimus: Fire hydrant exercise20, side – stepping with theraband, standing and abduction of leg with theraband, side lying position and abduction of leg with theraband for 2 sessions/week for a period of eight weeks (three sets of 10 repetitions).
Gluteus maximus strengthening : bilateral bridge, unilateral bridge and non-weight -bearing hip extension in prone with the knee flexed at 90 degrees for 2 sessions/week for a period of eight weeks (three sets of 10 repetitions)22.
Outcome
Measures: Numeric Pain Rating Scale (NPRS) and
Star Excursion Balance Test (SEBT).
RESULTS
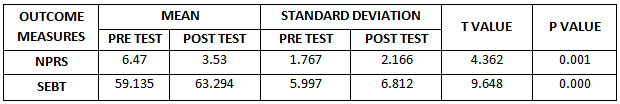
Group A (Control Group)
Table 1. Paired t test within Group A on Numeric Pain Rating Scale and Star Excursion Balance
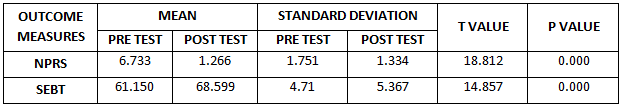
Group B (Experimental Group)
Table 2. Paired t test within Group B on Numeric Pain Rating Scale and Star Excursion Balance
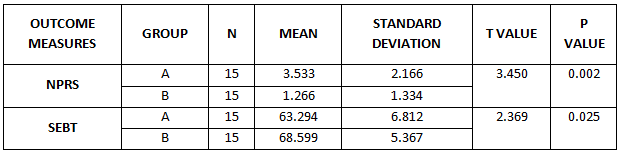
Comparison between Both Groups
Table 3. Comparison between Groups A and B on Numeric Pain Rating Scale and Star Excursion Balance
DISCUSSION
This study was conducted to investigate the effectiveness of gluteal muscle strengthening exercise in patients with plantar fasciitis. 30 subjects those satisfying the inclusion criteria were recruited for the study. Subjects were then allocated to two groups- Group A (control group) and Group B (experimental group), 15 in each group. Each subject was explained about the procedure of the intervention and the possible risks involved. A written informed consent from each subject was obtained. Subjects in group A received conventional treatment and subjects in group B received experimental treatment of gluteal muscle strengthening exercises and conventional stretching exercise. All subjects well tolerated the interventions given and no one was dropped out of the study.
Pain and lower limb functions were measured using reliable tools. Pain was measured using Numeric Pain Rating Scale (NPRS) and lower limb functions were measured using Star Excursion Balance Test. All outcome measures were collected before and after the intervention protocol. In both groups paired t- test was used to compare the pre and post test values. The post test scores of both groups were analyzed using two sample t test.
The results of the study after intervention of 2 months of gluteal muscle strengthening and conventional stretching exercises, patient had reduction in pain and improvement in lower limb function.
Plantar fasciitis is characterized by localized inflammation of plantar fascia and perifascial structures. It is a condition with an etiology of faulty biomechanics of lower limb musculature20. Gluteus medius and gluteus minimus plays the role of primary abductors of hip17. Weakness of the gluteus maximus results in decreased strength of hip extension and lateral rotation. The hamstring muscle plays a compensatory role in case of weak hip extensors and this leads to tightness of hamstring thus causing an increase in knee flexion24. All these together may cause prolonged forefoot loading makes plantar fascia more prone to injury. It causes plantar heel pain and functional disability. Therefore there is a need for strengthening in patients with plantar fasciitis who experience gluteal muscle weakness and increased heel pain. So, this study used intervention protocols which include gluteal muscle strengthening exercise along with conventional stretching exercises in patient with plantar fasciitis.
Studies have reported the effect of stretching with and without muscle strengthening exercise for the foot and hip in patients with plantar fasciitis, a single randomized controlled single blind trial, patients with plantar fasciitis allocated to one of the three treatment options for an eight week period: foot exercise group (extrinsic and intrinsic foot muscles), foot and hip exercise group (abductor and lateral rotator muscles) and stretching alone exercise groups and they concluded all three exercise protocols analyzed led to improvements at eight week follow-up in pain, function and dynamic lower limb stability in patients with plantar fasciitis21. “Combination of hip strengthening and manipulative therapy for the treatment of plantar fasciitis: a case report was concluded that the combination of hip strengthening and manipulative therapy improved foot pain in a patient with clinical diagnosis of plantar fasciitis 1.
Effects of hip strengthening exercise in a patient with plantar fasciitis and they concluded that the 3 month follow-up revealed that the heel pain and pelvic pain did not occur in the long distance walking, and there was no pain and discomfort at one year follow up. These above mentioned studies suggest that weakness of hip muscles is closely related to the etiology of plantar fasciitis. The result of the present study support the above studies that are gluteal muscles play an important role in the plantar fasciitis25.
The objectives of NPRS and SEBT was used in the study, NPRS provide standardized, quantitative description of pain and SEBT provide quantitative description of lower limb function in patients with plantar fasciitis before and after the interventions in group A and group B.
The objective of using NPRS in this study before and after the intervention in Group A (control) and group B (experimental) was that it is one of the most valid outcome measure for measuring pain. Based on the statistical analysis in experimental group, pre test mean value with standard deviation of NPRS was 6.733 ± 1.751 and of post test mean value with standard deviation of NPRS was 1.266 ± 1.334, degree o freedom was 14, t value was 18.812 and correlation was 0.766. The result shows that this is a significant difference between the pre NPRS values and post NPRS values at 5% significance level.
Based on the statistical analysis in control group (Group A), the pretest mean value with standard deviation of NPRS was 6.47 ± 1.767 and of the post test mean value with standard deviation of NPRS was 3.53 ± 2.166, degrees of freedom was 14, t value was 4.362 and correlation was 0.135. The results show that there is significant difference between the pre NPRS values and post NPRS values at 5 % significance level.
While comparing group A and group B, the mean of NPRS score of group A was 3.533 and of group B was 1.266. The standard deviation of group A was 2.166 and of group B was 1.334, t value was 3.450 and degree of freedom was 28. The result of the study shows that there is a statistically significant difference between post NPRS values of control and experimental group. The post test mean of NPRS shows that experimental group (Group B) shows significant reduction in pain in patients with plantar fasciitis than in control group (Group A).
The objective of using SEBT in this study before and after the intervention in group A and group B was that it is one of the most valid outcome measures for measuring the lower limb function. Based on the statistical analysis in experimental group (GroupB), the pre test mean value with Standard deviation of SEBT was 61.150 ± 4.71 and of post test mean value with standard deviation of SEBT was 68.599 ± 5.367, degrees of freedom was 14, t value was 14.857 and correlation was 0.934. The results show that there is significant difference between pre SEBT and post SEBT values at 5% significance level.
Based on the statistical analysis in control group (Group A), the pre test mean value with Standard deviation of SEBT was 59.135 ± 5.997 and of post test mean value with standard deviation of SEBT was 63.294 ± 6.812, degrees of freedom was 14, t value was 9.648 and correlation was 0.974. The result shows that there is significant difference between pre SEBT value, and post SEBT value at 5% significance level.
While comparing group A and group B, the mean of SEBT score of group A was 63.294 and of group B was 68.599, standard deviation of group A was 6.812 and of group B was 5.367, degrees of freedom was 28 and t value was 2.369. The result of the study shows that there is a statistically significant difference between SEBT scores of both groups at 5% significance level. The post test mean value of SEBT shows that experimental group (Group B) has significant improvement in lower limb function in patients with plantar fasciitis than in the control group (Group A ).
Due to the important role of gluteal muscles in hamstring tightness the protocol that involved the strengthening of the gluteal muscles were expected to lead to greater improvement in pain and lower limb function. However the result showed that gluteal muscles strengthening in addition to the conventional stretching exercises reducing the plantar heel pain and improved the lower limb function. Gluteal muscle strengthening exercise in addition to stretching exercise may increased the strength of gluteal muscles and thereby increased hamstring muscle length (Arab et al)39 which corrected the prolonged forefoot loading and discouraged the windlass mechanism thus correcting the faulty biomechanical etiology of plantar fasciitis.
It will be more accurate if the study is conducted with long duration and more number of sample size. The comparison between the prevalence of PF in males and females can also be attempted. An assessment of strength of gluteal muscles and hamstring muscles can give accurate results. Further studies are required with more sample size and more study duration to get the long term effects of the experimental intervention. Future research should also attempt to evaluate the strength of gluteal and hamstring muscles to prove the biomechanical changes occurring in the lower limb.
Ethical Clearance: Ethical clearance has obtained from CPAS School of Medical Education, Gandhinagar, Kottayam, Kerala.
Conflict of interest: There was no conflict of interest to conduct this study.
Fund for the study: It was aself financed study.
CONCLUSION
The result of the study showed that gluteal muscles strengthening exercises along with conventional treatment is more effective than conventional treatment alone in reducing pain and improving lower limb function in patients with plantar fasciitis.
Based on the statistical analysis, post test mean with standard deviation of NPRS in experimental group was 1.266±1.334 and post test mean with standard deviation of SEBT in experimental group was 68.599±5.367. Post test mean with standard deviation of NPRS in control group was 3.533±2.166 and post test mean with standard deviation of SEBT in control group was 63.293±6.812. The result showed that there was improvement in lower limb function and reduction in pain after application of intervention in the experimental group and control group.
Also the result of the study shows that there is a statistically significant difference between experimental group and control group supporting the hypothesis.
After analyzing the study it can be concluded that gluteal muscles strengthening exercises helps in improving lower limb function and reduction in pain in patients with plantar fasciitis. Therefore the study rejects the null hypothesis and accept alternate hypothesis
REFERENCES
- Santos BD and et al. (2016). Combination of Hip Strengthening and Manipulative Therapy for the Treatment of Plantar Fasciitis: A Case Report. J Chiropractic Med., 15(4); 310-313.
- Labovitz Jonathan M, Yu Jenny , Kim Chul (2011).The Role of Hamstring Tightness in Plantar Fasciitis.Foot and Ankle Specialist .; 4; 141-144.
- Lori A. Bolgla, Terry R. Malone (2004). Plantar Fasciitis and the Windlass Mechanism: A Biomechanical Link to Clinical Practice.J Athl Train. 39(1); 77-82.
- Crawford F, Atkins D, Edwards J. (2002). Interventions for treating plantar heel pain. Foot. 11; 228-250.
- Gudeman SD, Eisele SA, Heidt Jr RS, Colosimo AJ, Stroupe AL (1997). Treatment of plantar fasciitis by iontophoresis of 0.4% dexamethasone: a randomized, double-blind, placebo-controlled study. Am J Sports Med., 25; 312-316.
- Mc Poil T, Martin R, Cornwall M, Wukich D, Irrang I, Godges J, et al. (2008). Heel pain- plantar fasciitis- clinical practice guidelines linked to the international classification of function disability and health from the orthopedic section of the American physical therapy Association J Orthop Sports Phys Ther., 38; A1- 18.
- Cotchett M, Lennecke, Medica VG, Whittaker GA, Bonanno DR. (2017). The association between pain catastrophising and kinesiophobia with pain and function in people with plantar heel pain. Foot (Edinb)., 32:8-14.
- Whiting WC, Zernicke RF. (1998). Lower-extremity injuries. In: Biomechanics of Musculoskeletal Injury. Champaign, IL: Human Kinetics, 172–173.
- Monteagudo M, et al. (2018). Plantar Fasciopathy: A current concepts review. Efort Open Rev. Aug 29; 3(8); 485-493.
- Beeson P. (2014). Plantar Fasciopathy: Revisiting the risk factors. Foot Ankle Surg; 20; 160- 165.
- Scher DL, Belmont PJ Jr, Bear R, et al. (2009). The incidence of plantar fasciitis in the United States military. J Bone Joint Surg. Am., 91; 2867-2872.
- Frey C, Zamora J. (2007). The effects of obesity on orthopaedic foot and ankle pathology. Foot Ankle Int., 28; 996-999.
- Mc Clinton S, Weber CF, Heiderscheit B. (2018). Low back pain and disability in individuals with plantar heel pain. Foot( (Edinb)., 34; 18-22.
- Wolgin M., Cook C., Graham C., Mauldin D. (19940. Conservative treatment of plantar heel pain: long-term follow-up.Foot Ankle Int., 15; pp. 97-102.
- Martin R.L., Irrgang J.J., Conti S.F. (1998). Outcome study of subjects with insertional plantar fasciitis.Foot Ankle Int ; 19; pp. 803-811.
- Beyzadeoglu T., Gokce A., Bekler H.(2007). The effectiveness of dorsiflexion night splint added to conservative treatment for plantar fasciitis.Acta orthopaedica et traumatologica turcica., 41; pp. 220-224.
- Oatis Carol A. (2004). The mechanics of human movement. 2nd ed. Baltimore: Lippincott Williams & Wilkins; 6; Hip unit; 686-726.
- Harty J, Soffe K, O’Toole G, Stephens M M. (2005). The role of hamstring tightness in plantar fasciitis. Foot Ankle Int. 26; 1089-1092.
- Fuller EA. (2000). The windlass mechanism of the foot. A mechanical model to explain pathology. J Am Podiatr Med Assoc.;90(1); 35-46.
- Kwong PK, Kay D, Voner PT, White MW. (1988). Plantar fasciitis: mechanics and pathomechanics of treatment. Clin Sports Med.; 7; 119-126.
- Kamonseki DH, Gonçalves GA, Yi LC, Júnior IL. (2015). Effect of stretching with and without muscle strengthening exercises for the foot and hip in patients with plantar fasciitis: a randomized controlled single-blind clinical trial. Man Ther., 23; 76-82
- . Martin RL, Davenport TE, Reischl SF. (2014). Heel pain-plantar fasciitis, J Orthop Sports Phys Ther., 44(11); A1–33.
- Bolivar YA, Munnuera PV, Padillo JP. (2013). Relationship between tightness of posterior muscles of the lower limb and plantar fasciitis. Foot Ankle.
- Jonkers I, Stewart C, Spaepen A. (2003). The complementary role of the plantarflexors, hamstrings and gluteus maximus in the control of stance limb stability during gait. Gait Posture.,17(3); 264-272.
- Lee JH, Park JH, Jang WY. (2019). The effects of hip strengthening exercises in a patient with plantar fasciitis: A case report. Medicine (Baltimore)., 98(26); e16258.
| Citation: Jomi John, Jince Augustine (2020). Effectiveness of gluteal muscles strengthening in patients with plantar fasciitis, ijmaes; 6 (2); 740-748. |