| Lucky Anggiat1, Wan Hazmy Che Hon2, Siti Nur Baait binti Mohd Sokran3, Nurul Mawaddah Binti Mohammad3 |
| Author: 1Faculty of Vocational Studies, Physiotherapy Program, Universitas Kristen Indonesia, Jakarta, Indonesia 3School of Health Sciences, KPJ Healthcare University College, Nilai, Malaysia Corresponding Author: 2Consultant Orthopaedic Surgeon, KPJ Seremban Specialist Hospital and KPJ Healthcare University College, Jalan Toman 1, Kemayan Square, 70200 Seremban. Email address: whazmy@hotmail.com |
ABSTRACT
Background of study: Non-specific low back pain (LBP) becomes the most common cases in University population. Prolonged sitting has been identified as one of the factors leading to non-specific LBP among University population. The purpose of the study is to identify the change of functional disability in non-specific LBP among university population after PNF and McKenzie method.
Methods: A quasi-experimental study involving 36 subjects (students and office workers) from the university population. The study population were selected from students and office worker of KPJ Healthcare University College (KPJUC) who met the inclusion criteria. The subjects were divided into three treatment groups: PNF group, McKenzie group and control group (hot pack and educational home exercise sheet) which underwent 12 treatment sessions distributed over three times in a week for four weeks duration. Subjects were measured on functional disability by Oswestry Disability Index (ODI). Measurement was performed at pre-test, mid-test and post-test. Repeated measures ANOVA was used to analyse the effectiveness of PNF and McKenzie treatments based on the measurement time.
Result: This study showed that the PNF and McKenzie gave effect in improving ODI score in within group analysis. However, the results of PNF showed that it has more effect than McKenzie method on functional disability score (p <0.05) after 4 weeks.
Conclusion: There was a change in functional disability on non-specific LBP after PNF and McKenzie method. Furthermore, the study findings showed that the PNF exercise has more effect in improving functional disability compared to McKenzie method on non-specific LBP among university population.
Keywords: Functional Disability; Mckenzie; Non-Specific LBP; PNF
| Received on 10th February 2020, Revised on 19th February 2020, Accepted on 24th February 2020 |
DOI:10.36678/ijmaes.2020.v06i01.001
INTRODUCTION
Low back pain (LBP) consists of two types, which is specific and non-specific LBP. Specific back pain can further be divided into LBP which that is related with vertebrae and non-vertebrae. The non-specific LBP is developed from the soft tissue, which is poorly localised 1. In addition, non-specific LBP is further classified into LBP, which is not related to the neurological problem and degenerative syndrome. Prolonged sitting led to increased body discomfortness in the neck, shoulder, upper back, low back, and buttock while prolonged slumped sitting may be related to Internal Oblique or Transverse Abdominis muscle fatigues—compromising the stability of the spine, making it vulnerable to injury 2.
University population mainly consists of students, office workers and academicians, which have similar habit to experience prolonged sitting. Students usually attend the classroom session for learning theories and at the same time working in front of computer to browse some resources. They experience prolonged sitting in most of their daily activities. A previous study conducted by Nordin, Devinder, and Kanglun reported 31% of students usually sat in the classroom or worked daily in front of the computers everyday for 6 to 8 hours 3.
Similarly, majority of the office workers working in the university, sit more than 4 hours daily with 90.8% prevalence while other office workers who sit in the same working position usually leave their office chair only for 10 minutes or less each day have scored about 65.8% prevalence. Prolonged sitting is one of the factors causing musculoskeletal pain among university population, which are student and office worker, who experienced from having LBP (LBP), which commonly reported 4.
A study conducted by University in Columbia found that 45% of the university population were having severe chronic pain specifically in the lower back region. A study by Nordin, Devinder, and Kanglun; also revealed similar results which stated that 64.6% of students had LBP and it was found that the students also sat in the classroom or worked in front of the computers everyday between 6 to 8 hours 5,6.
Some anatomical condition related to those factors can be contributed to the incidence of LBP. Low back pain may developed by some factors which increase lumbar lordosis, reduce abdominal muscle length and strength, and decrease back extensor muscle endurance, back extensor muscle flexibility, length of iliopsoas, hamstring muscle flexibility, body composition and others 7,8.
A study by Casas et al. found that the prevalence of limitation for academic activities was almost 30% and it affected to both office workers and students on their daily life activities. It caused potential effects to the life quality of both the office workers and the students. The limitation in academic activities due to pain was 29.8%. The researchers concluded that there was moderate disability due to LBP among physiotherapy students in Mumbai 9.
The similar potential risk happened to office workers who were suffering from LBP. An employee with LBP usually took a day off from his work for medical check-up would decrease the company’s productivity if it had a significant number of employees who were absent from work due to having LBP. The impact of LBP on physical activities does not only depend on the pain but also on some functional disability, which is inter-related one to another 10,11.
There are several options and suggestions on the treatment to reduce LBP in the population . Exercise is also one of the physiotherapy treatments that can strengthen the muscle that supports the spine 12,13.
Theraphy exercise was found to be the best choice to reduce LBP and to increase body functions in adult people who experienced LBP. The therapeutic exercise for LBP uncommonly performed by physiotherapist called Proprioceptive Neuromuscular Facilitation (PNF), however; this treatment is commonly used for neurological conditions 16,17.
PNF has been recommended for sensory-motor control training, as well as for stimulating lumbar muscle proprioception. Kofotolis and Kellis stated in their study that PNF significantly improve the muscle endurances. They defined that the Rhytmical Stabilization (RS) exercise provided the trunk static endurance and Combination of Isotonic (COI) provided dynamic muscle endurance 18,19.
In other studies, in comparing modalities of therapy exercises, PNF was shown to have better result than manual therapy, core stability exercise and ball exercise for LBP which was commonly used for the trunk muscle, pelvic stability, and core muscle 20, 21.
A common therapy exercise used for LBP was developed by Brian McKenzie, which was recognised as McKenzie method. A systematic review study has shown that McKenzie therapy is more effective than the comparred treatment at short-term follow up for spinal pain. The comparative treatments in these trials include Non-Steroid Anti Inflammation Drugs (NSAIDs), educational booklet, back massage with back care advice, strength training and spinal mobilization and general mobility exercises. McKenzie method can be a familiar treatment and it is one of the common choices used by most physiotherapists for treating LBP 22,23.
There were several studies that performed the specific exercises to treat LBP, such as McKenzie method, PNF, ball exercise, yoga, spinal stabilization exercise, Mat based Pilates and ordinary exercise that is aerobic exercise which is effective and it has a good result for LBP. However, these previous studies did not conduct any comparison between PNF exercise and McKenzie method to verify the effect of each treatment. Therefore, this study carried out the changes of functional disability among university population after the PNF exercise and McKenzie method and specifically comparing the effects of those treatments 24,25.
METHODOLOGY
This was an experimental study using quasi-experimental study. Quasi-experimental study is defined as study comparing the effect and value of intervention in between three groups at their pre-test, mid-test and post-test design in which subjects are equally differentiated on the treatment given and on the control group. All subjects that included in this study were assigned to three groups. Upon selection, subjects were given written and verbal study information and informed consent, which states that they are willing to be the subject of this research. Informed concent received from all subjects then physiotherapist assessed the subject based on the measurements called disability score using Oswestry Disability Index (ODI). In addition, the information about age, gender, occupation and years of working or studying were collected and presented as socio-demographic data of the subjects.
The three groups of subjects, who had been managed with PNF exercise, McKenzie method and control group respectively, were compared. The assessment point was performed at three points; pre-test as the baseline measurement, mid-test was given two weeks after treatment and post-test as the last measurement after four weeks treatment. The subjects had to undergo 12 sessions of treatment, 3 sessions in each week of four-week-treatment. This study was conducted in a private academic institute and the ethical approval has be obtained from School of Health Sciences, Research Management Centre, KPJ Healthcare University College (KPJUC), in Nilai, Negeri Sembilan, Malaysia before starting the study.
The inclusion criteria were the subjectssuffering from chronic non-specific LBP. Chronic non-specific low back pain was determined based on the subjects’ report. The physiotherapist conducted the assessment to make sure the low back pain was non-specific in nature 3, 4. All subjects were also asked about their duration of sitting in a typical working day because prolonged sitting is one of the contributing factors for non-specific low back pain with age ≥ 18 to 45 years old 26, 27.
Participants were excluded in this study according to the exclusion criteria, which are subjects with any history of pathological conditions or diagnosed with disk herniation, spinal stenosis, spondylolisthesis, spondylitis, radiculopathy, vertebral fracture, surgery to lumbar spine, reported with pregnancy and reported with other medical illnesses such as tumour, kidney disease, and visceral disease 28.
The subjects were 36 subjects and the office workers
of KPJUC who met the selection criteria prior to sample screening. The determination of the sample size was done using G*power 3. The three groups used F test, the effect size f was 0.25 and power was 0.8. Based on the data, the calculated total sample size is thirty and as additional subject is 20% from total sample size, which is six and therefore, the total sample size were thirty-six with twelve subjects for each group. The sample size was determined based on a previous study.The timing for the implement-tation of data collection and testing of the research subjects was from August 2017, December 2017.
Three of the physiotherapists participating in this study were trained by the principal physiotherapist to perform the specific PNF exercise and McKenzie method used as experimental treatment in this study. The training includedwith visual demonstrations, hands-on experience and technique evaluation. The training was continued until all physiotherapists had successfully mastered each technique. Physiotherapists performing the PNF exercise and McKenzie method reached the training criteria within two-week period. In addition, these three physiotherapists were closely supervised by the principal physiotherapist in charge in KPJUC Rehab Centre to assure proper performance of PNF exercise and McKenzie method for the techniques and the assessment of the subjects.
Measuring Tools: The Oswestry Disability Index (ODI) was used to assess the subject’s disability that caused by the non-specific LBP. The questionnaire contains 10 sections, with six statements for each section. The questionnaire can be self-administered by the patient or assessed by the physiotherapist; it is usually completed in less than five minutes and scored in less than one minute 29.
Each subject was asked to select one statement in each section of the questionnaire which best represents his or her perceived ability to perform a function and a quantity of pain experienced on the assessment day. Each statement is scored on a 6-point scale (0-5), where a score of “0” is awarded if the client selects the first statement of the section and a score of “5” is awarded if the client selects the last statement. The section scores are tallied to produce a total raw score. Total raw scores can vary from 0 to 50 and the percentage ranges from 0-100 30.
Intervention Procedures: Subjects in the group I received the PNF exercise intervention. The PNF technique was performed on the trunk movement. The patient was in a sitting position. First, the physiotherapist conducted the Rhythmic Stabilisation (RS). The RS exercise consisted of alternating (trunk flexion-extension) isometric contractions against resistance for 10 seconds, with no motion intended. The subjects performed three sets of 10 repetitions at maximal resistance provided by the same physiotherapist. The resting intervals of 30 seconds and 60 seconds were provided after the completion of 10 repetitions for each pattern and between sets, respectively. Secondly, the physiotherapist conducted combination of isotonic technique with flexion or extension for lumbar, depending on the patient condition. The combination of isotonic technique consists of alternating concentric and eccentric contractions of agonists without relaxation. The resisted active concentric contraction for 5 seconds, resisted eccentric contraction for 5 seconds, and resisted maintained during contraction for 5 seconds (trunk flexion-extension). The combination of isotonic performed three set of 10 repetitions with resting intervals of 30 second and 60 second were provided after completion of 10 repetitions for each pattern and between sets, respectively. Then, all PNF exercises will be held for 30-45 minutes 31.
The subjects in the group II received the McKenzie method treatment. The physiotherapist guided the subject to conduct four extension exercises and three flexion exercises. The extension exercise started with these following stages. Firstly, the subjects laid their face down for one until two minutes. Secondly, they laid their faces down with extension. The subject were asked to start laying their faces into down position followed by the extension of the trunk on the elbow and held on for five seconds and went back to the first position as a relaxation. Thirdly, extension on lying, the subjects were instructed to start lying their faces into down position, followed by the extension of the trunk with elbow extension (push-up position) for ten seconds, then the subject were asked to relax by going back to the first position. Forthly, extension on standing, the subjects were instructed to get standing position and then they were asked to do the extension of the trunk and to hold for five seconds with hands of the back and the fingers pointing backwards, followed by a relaxation by going back to the standing position. All extension exercise were repeated for ten repetitions in two sets.
The flexion exercise was started by these following steps. Firstly, flexion on lying, the subjects wereasked to get a lying position and asked to flex the trunk with both knees to the chest and to hold with both hands. Subjects were instructed to hold that position for five seconds and get a relaxation by going back to the first lying position. Secondly, flexion on sitting, the subject were asked to sit on the edge of a chair and instructed to bend the trunk forward and to grasp the ankle or to touch the floor with both hands. This position was maintained for five seconds and it was followed by a relaxation to the first position. Thirdly, flexion on standing, the subjects wereasked to get a standing position, then instructed to bend forward or to flex the trunk with fingers down to the legs as far as the subjects comfortably reach them. The subjects wereasked to hold on the last position for five seconds and asked to go back to a standing position as a relaxation. Then, all flexion exercise was also repeated for ten repetitions in two sets. There were three minutes for resting intervals in every set. The McKenzie treatment lasted for 20-40 minutes 30.
The subjects in the group III were treated using hot pack for 15 minutes as a basic treatment for non-specific LBP. The physiotherapist gave them some home exercises guided by educational exercise sheet and teach the subjects how to use it. A narrative review, written by Bardin, King and Maher , revealed that a hot pack considered as the first line of care for non-specific LBP along with self-management with home exercise. The exercise based on the educational exercise sheet lasted for 7-10 minutes that can be done at home or the office. All of the subject in each group underwent 12 sessions of treatment, 3 sessions in each week of a four-week-treatment.
Data analysis: All data analysed were performed by using IBM SPSS Statistics for Windows, Version 22.0. Repeated measures ANOVA analysis were used to determine the result of differences before and after treatment given in every group. Repeated measure ANOVA within-between groups analysis were applied to determine the effect between three treatment groups based on time measurement. Bonferroni adjustment were applied for multiple comparison.
RESULT
The total number of subjects of 36 was divided into 3 treatment groups, and each group consisted of 12 subjects. Most of the participants were 18-25 year-old subjects (75%), female (63.9%), and students (61.1%) who had been studying or working for 1-3 years (75%). The socio-demographic details such as age, gender and occupation are tabulated in Table 1.
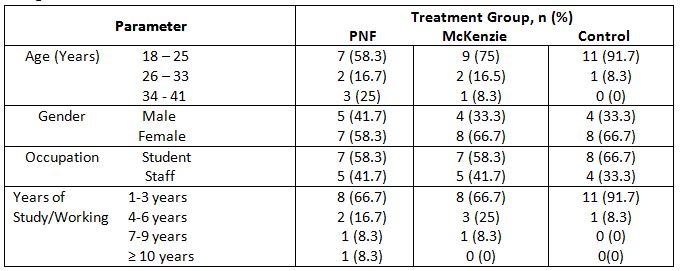
Table 2 described the within group result of PNF exercise, McKenzie and Control group using Oswestry Disability Index (ODI) in terms of Mean Difference (MD) and Confidence Interval (CI). There was a significant effect of time on ODI F = 97.91, p = 0.001.
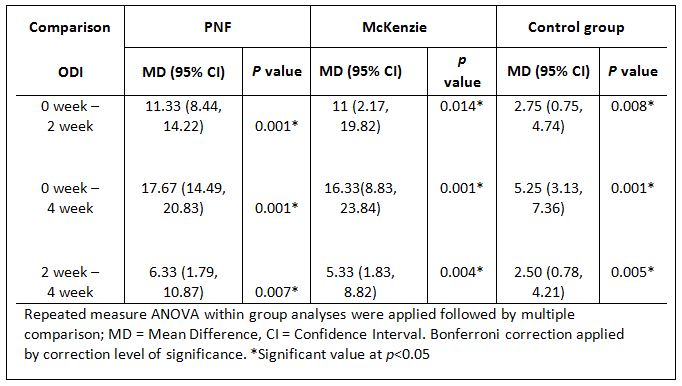
Table 3 below describes between group result of PNF exercise, McKenzie and Control group in Oswestry Disability Index (ODI) in terms of Mean Difference (MD) and Confidence Interval (CI). There was significant difference of ODI score between the group (F= 6.19, p = 0.005).
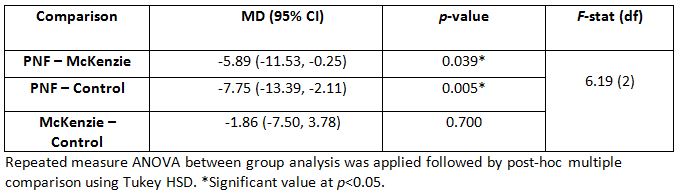
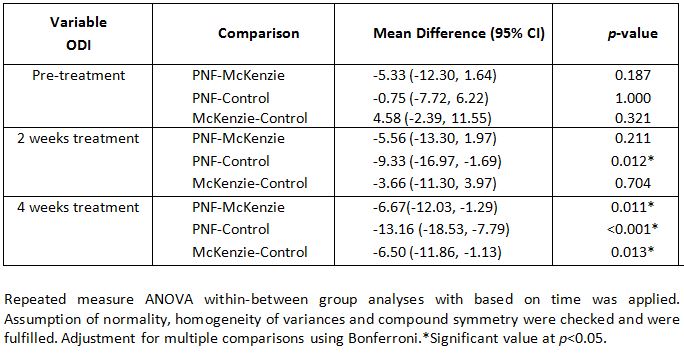
Table 4 describe the comparison between PNF exercise with Control group, McKenzie method and Control group treatment on ODI in terms of Mean difference and p-value for every comparison group. The Multivariate test for ODI-treatment interaction result based on F-test showed the p < 0.005.
DISCUSSION
The findings of the present study showed that there was a good improvement in functional disability that was assessed by using Oswestry Disability Index (ODI) in within group analysis. Those three treatments showed significant result in reducing the ODI score after treatments both after 2 weeks and after 4 weeks. This implied that all the three treatments were successful in reducing the ODI score. In between groups and time-treatment interaction, showed there was significant difference result in increasing ODI score by PNF than control group treatment after 2 weeks of treatment, however, comparison between PNF and McKenzie showed no significant difference so as between McKenzie and control group comparison. After 4 weeks treatment, PNF showed more statistically significant difference in reducing the ODI score than the McKenzie group and extremely significant difference than the control group. Although, the McKenzie also showed significant difference in reducing the ODI score than control group, it could be implied that the PNF exercise was superior to the McKenzie and control group 31.
The result of this present study was also supported with the findings of the study by Kumar, Zutshi and Narang, who reported that PNF showed significant improvement in ODI score compared with conventional exercise for LBP that consist of knee to chest, pelvic bridging, pelvic rolling and alternate arm leg extension after 4 weeks. This study also revealed that PNF showed better result in muscle endurance test, which can be concluded the improvement in muscle endurance test can contribute in reducing the ODI score result after the PNF exercise. Thus, prolonged sitting activity which was one of the habits in the present study population contributed to reduction in trunk muscle endurance 32.
Sawant and Ghodey studied on PNF functional ability and trunk muscle endurance which confirmed that PNF has shown significant improvement in trunk muscle endurance and functional ability with ODI on chronic mechanical LBP patient. The study on the effectiveness of PNF for LBP done by Franklin et al. reported that the PNF showed highly significant difference to improve the ODI score compared with core stability exercise. The PNF exercise in this previous study underwent 4 weeks session at the same period with core stabilisation exercise 33.
Similar study conducted by Dhaliwal et al. [36] regarding to PNF program versus core stabilisation exercise for decreasing pain and improving function on patient with LBP, reported that the PNF significantly decrease the ODI score among patient with LBP. Thus, those previous studies strengthened the facts that PNF is better in strengthening of the core muscle than the core stability exercise, with further improvement in the functional ability outcomes of LBP. The results from previous studies also implied that the PNF, compared with core stabilisation exercise, were better in reducing the ODI score and supported the present study result. Another study comparing the PNF with conventional strengthening exercise, which consist of exercise for transversus abdominis muscle and multifidus showed that PNF gave better improvement in ODI score than the conventional exercise 34.
The exercise period in their study was only for 3 weeks, which can be implied that the PNF could be improving the ODI score even before 4 weeks. As McKenzie focusing more on postural correction and not on providing the core strength exercise, it can be concluded that the PNF was more superior in reducing the ODI score with improved trunk muscle endurance than McKenzie method.
This study had several limitations. Firstly, the sample size was small, leading to reduced statistical power. Secondly, even though the result revealed there are statistically significant, the difference score of ODI did not meet the minimal clinically important. Future study is required to meet minimal clinically important score of ODI. The McKenzie method was followed the Treat your Own back booklet from McKenzie which not the proper Mechanical Diagnosis and Treatment (MDT), however, the results showed the McKenzie method have a good effect to subjects. Future study also needed to compare the MDT with PNF properly.
Since this study was conducted to determine the direct impact of the treatment, it could not be guaranteed for the treatment to produce better effects if the follow-up sessions are extended, which the present study does not assess on the long-term effects. This present study used a quasi-experimental design, thus the development of study design for future study is also suggested in improving the level of other studies.
The researchers recommended using PNF exercise for the physiotherapist in order to get better outcome for non-specific LBP patient. Furthermore, as a prevention and self-management for the patients which are engaged in a prolonged sitting, the physiotherapist can provide them with educational exercise sheet and McKenzie method for home exercise program besides their regular treatment with physiotherapist.
Ethical Clearance: Received approval letter from the Research Ethics Committee, School of Health Sciences, KPJ Healthcare University College with reference number: KPJUC/RMC/ MPT/ EC/ 2017 /89 dated 02/08/2017.
Fund for the study: Research Management Center, Department of Physiotherapy, School of Health Sciences, KPJ Healthcare University College, Malasia.
Conflict of Interest: All authors have no conflict of interest to declare on conduct of this study.
CONCLUSION
This study revealed that the three treatments made change on ODI score in each group analysis. However, further comparison between PNF exercise and McKenzie method showed that PNF exercise has more effect in improving the functional disability score than McKenzie method on patient with Non-specific LBP.
Acknowledgement: We would like to thank the Research Management Center, Department of Physiotherapy, School of Health Sciences, KPJ Healthcare University College, for all the physiotherapists and all the facilitators. Lastly, we extend our gratitude to all those who participated in this study.
REFERENCES
- Taguchi, T. (2003). Low back pain in young and middle-aged people, Journal of Japan Medical Association; 46(10); 417–423.
- Waongenngarm, P., Rajaratnam, B. S., & Janwantanakul, P. (2016). Internal Oblique and Transversus Abdominis Muscle Fatigue Induced by Slumped Sitting Posture after 1 Hour of Sitting in Office Workers. Safety and Health at Work; 7(1); 49-54.
- Nordin, N. A., Devinder, A. S., & Kanglun, L.(2014). Low Back Pain and Associated Risk Factors among Health Science Undergraduates. Sains Malaysiana 43(3); 423-428.
- Janwantanakul, P., Sihawong R., Sitthipornvorakul E., Paksaichol, A.(2015). A screening tool for non-specific low back pain with disability in office worker : a 1 year prospective cohort study. BMC Musculoskeletal Disorders; 16 : 298.
- Mozafari, A., Vahedian, M., Mohebi, S., Najafi M. (2015). Work-related Musculo-skeletal disorder in truck drivers and office worker. Acta medica Iranica; 53: 7.
- Koley S, Kaur J, Sandhu JS.(2010). Biological risk indicators for non-specific low back pain in young adults of Amritsar, Punjab, India. Journal of Life Sciences; 2: 43-48.
- Koley S, Sharma L, Kaur S.(2010). Effects of occupational exposure to whole body vibration in tractor drivers with low back pain in Punjab. Anthropologist; 12: 183-187.
- Patil, V.S., Master, M.F., Naik, R.V.(2016). A cross-sectional observational study on the prevalence of mechanical low back pain in physiotherapy students. National Journal of Intergrated Research Medicine; 7(6): 9-12
- Castellini, G., Gianola, S., Banfi, G., Bonovas, S., & Moja, L.(2016). Mechanical low back pain: Secular trend and intervention topics of randomized controlled trials. Physiotherapy Canada; 68(1): 61-63.
- Koes B, W., van Tulder M., Lin, C., Macedo, L, G., McAuley J., Maher C. (2010). An update overview of clinical guidelines for the management of non-specific low back pain in primary care. European Spine Journal; 19; 2075-2094.
- Gordon, R., Bloxham, S. (2016). A Sytematic review of the effects of exercise and physical activity on non-specific cronic low back pain, Healtcare journal; 4 : 22; 10.3390.
- Scharrer M, Ebenbichler G, Peiber K, Crevenna, Gruther W, Zorn C, Grimm- Steiger, Herceg M, Keilani M, Ammer K.(2012). A systematic review on the effectiveness of medical training therapy for subacute and chronic low back pain. European Journal Phyhsical Rehabilitation Medicine; 48: 361-70.
- Westwater-Wood, S., Adam N., Kerry, R. (2010). The use of proprioceptive neuromuscular facilitation in physio-therapy practice. Physical Therapy Reviews; 15(1).
- Lee YJ.(2009). The effects of the PNF Techniques on lumbar stability and the functional activity in chronic low back pain patients. Department of Physical Therapy Graduate School of Dongshin University,; pp 1–60.
- Kofotolis, N., Kellis, E.(2006). Effect of two 4-week proprioceptive neuromuscular facilitation programs on muscle endurance, flexibility, and functional outcomes performance in women with chronic low back pain. Physical Therapy; 86 (7): 1001-1012.
- Park, S. E., Wang, J.S.(2006). Effect of joint mobilization KEOMT and PNF on a patient with CLBP and a lumbar transitional vertebra : a case study, Journal of Physical Therapy Sciences, 2015; 27 : 1629-1632.
- Lee, C.-W., Hwangbo, K., & Lee, I.-S.( 2014). The effects of combination patterns of proprioceptive neuromuscular facilitation and ball exercise on pain and muscle activity of chronic low back pain patients. Journal of Physical Therapy Science; 26(1): 93-6.
- Kumar A., Zutshi K,. Narang N. (2011). Efficiacy of Trunk Propioceptive Neuromuscular Facilitation Training on Chronic Low Back Pain. International Journal of Sports Science and Engineering; 5 (3): 174-180
- Johnson GS., Johnson VS. (2002). The application of the principles and procedures of PNF for the care of lumbar spinal disabilities. The journal of manual and manipulative therapy; 10(2); 83-105
- Clare H, Adams R and Maher CG.(2004). A systematic review of efficacy of McKenzie therapy for spinal pain. Australian Journal of Physiotherapy; 50; 209-216.
- Garcia, A.N., Gondo, F.L.B., Costa, R.A., Cyrillo, F.N., Costa, L.O.P.(2011). Effects of two physical therapy interventions in patients with chronic non-specific low back pain : feasibility of a randomized controlled trial. Revista Brasileira Fisioterapia, Sao Carlos; 15(5): p.420-7
- Young, K. J., Je, C. W., & Hwa, S. T. (2015). Effect of proprioceptive neuromuscular facilitation integration pattern and swiss ball training on pain and balance in elderly patients with chronic back pain. Journal of Physical Therapy Science; 27(10): 3237–40.
- Casser HR, Seddigh S, Rauschmann M. (2016). Acute lumbar back pain-investigation, differential diagnosis and treatment. Deutsches Ärzteblatt International; 113: 223 34.
- Issa LF,. Seleem NA,. Bakheit AM,. Baky AA,. Alotaibi AF.(2016). Low back pain among undergraduate student at Taif University- Saudi Arabia. International Journal of Public Health and Epidemiology ; 5(6), pp 275-284.
- Maher, C., Underwood, M., Butchbindee, R.(2017). Non-specific low back pain. Seminar, Lancet; 389: 736-47.
- Sihawong, R., Janwantanakul, P., & Jiamjarasrangsi, W.(2014). A prospective, cluster-randomized controlled trial of exercise program to prevent low back pain in office workers. European Spine Journal; 23(4); 786–793.
- Hasanpour-Dehkordi, A., Dehghani, A., Solati, K. (2017). A comparison of the effects of Pilates and McKenzie training on pain and general health in men with chronic low back pain: A randomized trial. Indian Journal of Palliative Care; 23: 36-40.
- Longo G, Loppini M, Denaro L, Maffulli N, Denaro V. (2010). Rating scales for low back pain. British Medical Bulletin 98; 81-144.
- Jadeja, T., Vyas, N., Sheth, M. (2015). To Study the effect of proprioceptive neuromuscular facilitation on back muscle strength, pain, and quality of life in subjects with chronic low back pain-an experimental study. International Journal of Physiotherapy; 2(5); 778 -785.
- Aziz, S., Ilyas, S., Imran S., Yamin F., Zakir A., Rehman A., Adnan S., Khanzada S. (2016). Effectivenes of Mc. Kenzie Exercise in Reducing Neck and Back Pain Among Madrassa Student. International Journal Physiotherapy; 3 (1): 78-85.
- Paatelma, M., Kiplikoski, S., Simonen, R., Heinonen, A., Alen, M., Videman, T. (2008). Orthopedic manual therapy, McKenzie method or advice only for low back pain in working adults : A Randomised controlled trial with one year follow-up. Journal of Rehabilitation Medicine; 40; 858-863.
- Sawant, R., Ghodey S. (2017). Added effect of proprioceptive neuromuscular facilitation on functional ability and trunk endurance in chronic low back pain patients. International Journal of Allied Medical Sciences and Clinical Research; 5(2): 480-486.
- Franklin, C.V.J., Kalirathinam, D., Palekar T., Nathani N. (2013). Effectiveness of PNF Training for Cronic Low Back Pain. IOSR Journal of Nursing and Health Science (IOSR-JNHS); 2: 41-52.
- George, A, J., Kumar D, K, U., Nikhil N.P. (2013). Effectiveness of trunk proprioceptive neuromuscular facilitation training in mechanical low back pain. International Journal of Current Research; 5(7); pp.1965-1968.
| Citation: |
Lucky Anggiat, Wan Hazmy Che Hon, et al (2020).The changes of functional disability in non-specific low back pain among university population after proprioceptive neuromuscular facilitation and mckenzie method , International Journal of Medical and Exercise Science, 6 (1): 656-667.

Leave a Reply