KANCHAN A. KATRE1 , VIJAYAKUMAR PUSHPARAJ 2 , JIBI PAUL3
Authors:
1 Faculty of Physiotherapy, P.E.S Modern college of Physiotherapy, Modern College road, Pune-5, Maharastra, India .
3 Faculty of Physiotherapy, DR.MGR.Educational and Research Institute, Velappanchavadi, Chennai,India
Corresponding Author:
2 Professor, Rajarajeswari College of Physiotherapy, Kambipura, Mysore Road, Bangalore, Karnataka, India. Mail id: vijayrrc@yahoo.com
ABSTRACT
Introduction: The objective of the study was to determine the effectiveness of Otago exercise program (OEP) and strength training program (STP) on lower limb strength and risk of fall among bilateral knee osteoarthritis patients and compare its effects.
Method: Subjects diagnosed with bilateral knee osteoarthritis were included and randomly assigned into group A ( N=20) and group B ( N=20). Subjects in Group A received otago exercise program and strength training program in group B. All the subjects were assessed with baseline and post intervention outcome measure for risk of fall with The Time up and Go test (TUG) and lower limb strength with 30-sec Chair Stand Test.
Result: This study shows that the mean score Inter-group analysis of time up go test (TUG) in between Otago Exercise Program and Strength Training Program group shows (p < 0.05) with significant improvement and with mean score of 30sec Chair Stand Test (30sec CST) on the Lower limb strength in between Otago Exercise Program and Strength Training Program group shows no significant improvement with p value of 0.0570 (p>0.05).In intra group analysis the time up go test shows significant result in OEP group but not in STP group and with the 30 – sec chair stand test showed significant result in both the groups.
Conclusion: The study showed that otago exercise program is effective in reducing the risk of fall and improving lower limb strength among bilateral knee osteoarthritis than Strength training program.
Keywords: Osteoarthritis , Otago exercise program, strength training program, time up and go test, 30-sec Chair Stand Test and risk of fall.
Received on 11th February 2019, Revised on 24th February 2019, Accepted on 28th February 2019
INTRODUCTION
Osteoarthritis (OA) is a prevalent disease characterized by structural changes in cartilage, bone, synovium, and other joint structures1. Osteoarthritis is estimated to be the eighth leading non-fatal burden of disease, accounting for 2.8% of total years of living with disability2. It is the most prevalent and disabling chronic diseases affecting the elderly causing progressive dysfunction of articular cartilage which results in impaired joint motions, severe pain, and disability3. The ageing process is accompanied by a decline in function of systems that are responsible for the control of balance 4.
Osteoarthritis of the knee is associated with disability due to pain, quadriceps dysfunction, and impaired proprioception. Quadriceps dysfunction in OA knee includes impaired proprioception, especially in the more extended knee joint positions; impaired ability to accurately and steadily control submaximal force and impaired eccentric strength5. These proprioceptive deficits may contribute towards reduced dynamic knee stability. The integrity and control of sensorimotor systems i.e. proprioceptive acuity and muscle contraction,are essential for the maintenance of balance and production of a smooth and stable gait.It has been established that proprioceptive acuity, joint movement and sense of resistance declines both with age and as a result of OA 6,7.
Pattern of muscle use changes as an individual ages8. Out of more than 400 risk factors for fall9, lower limb weakness and decreased balance are the two of the most easily modifiable risk factors. Fall rates increase with age10 and the frequency of fall is higher among women than men11. With the increasing age, approximately after the age of 60 years, a person’s physical ability, including gait speed,muscle strength,and balance, generally declines, so the incidence of fall and the severity of fall related complications increase 12,13,14.
Timed Up & Go Test (TUG) is a test for balance that is commonly used to examine functional mobility in community-dwelling, frail older adults with age group between 70–84 years15 and appears to be a valid method for screening for both level of functional mobility and risk for fall in community-dwelling elderly people16. Also the 30-sec chair stand test provides a reliable and valid indicator of lower body strength in generally active, community-dwelling older adults17.
Balance and gait training are important components of any exercise program aimed at decreasing the risk of fall among older adults, so any exercise program for older adults should include exercises to improve both strength and balance18. Evidence has shown that certain rehabilitation exercises such as the Otago exercise program and Fall Management exercise are effective in returning fall patients to normal functional movement if the patient adheres to the routine19.
The Otago Exercise Program (OEP) is a fall prevention program which addresses the risk factors of poor balance and lower limb weakness with an individually prescribed, home based strength and balance exercise program in older adults. There are only very few studies about Otago Exercise Program focusing on reducing fall risk in older adults having bilateral osteoarthritis of knee. Also few studies have stated that the Strength training of the lower limb muscle helps to improve physical performance and reduce disability along with improving the strength of muscles in the community-dwelling elders with bilateral osteoarthritis of knee22. But there are very few studies done for reducing the risk of fall in older adults with bilateral osteoarthritis of knee by using Otago exercise program. Hence, the main purpose of this study was to determine whether there is effect of Otago Exercise Program over strength training program for 8 weeks in reducing the risk of fall and improving leg strength in older adults having bilateral osteoarthritis of knee.
Objective of the study: The main objective of the study was to determine the effect of Otago exercise program and strength training program and compare the effectiveness Otago exercise program over strength training program on leg strength and risk of fall among bilateral knee osteoarthritis patients.
METHODOLOGY
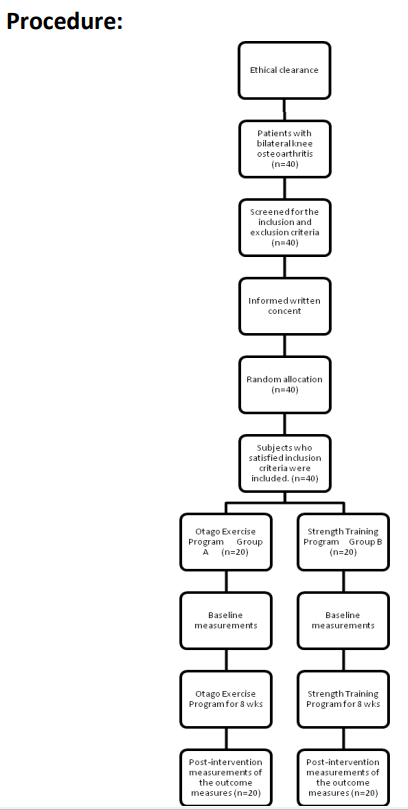
This was a randomized clinical trial study design conducted after obtaining the approval from the Institutional Ethical Committee (IEC) of PES Modern college of Physiotherapy, Pune. The subjects who reported to the outpatient department (OPD) of the study setting at PES Modern college of Physiotherapy, Pune with bilateral knee osteoarthritis were selected and screened for the inclusion and exclusion criteria. Those subjects who satisfied the inclusion criteria were included for the study. Total 40 subjects (n=40), of both male and female gender between age group of 60 to 69 years were included for the study and a written informed consent was obtained from each of the forty subjects, after explaining about the detailed procedure of the study. Then the selected subjects were randomly allocated into group A and group B with 20 subjects in each group. Group A ( N=20) received Otago Exercise Program (OEP) which contains strength training, balance training and walking program. Group B ( N=20) received Strength Training Program (STP), which contains only strength training. Each subject in both the groups received an exercise activity booklet of the respective exercise program, with illustrations and instructions about the program. All the subjects were instructed to wear comfortable clothing which should not be too tight or too loose while performing exercises. The subjects in each group were assessed for the baseline outcome measurement and post intervention outcome measurement with TUG test and 30 sec Chair Stand Test. The subjects in both the group were explained about the study and intervention in the language best understood by them. They were encouraged to clarify questions regarding the study if any. The baseline measures were recorded prior to intervention and post intervention measurements were recorded 8 weeks after intervention.
After obtaining the baseline measurement and during each session from day one, subjects in both groups were given a common treatment with Interferential Therapy with the frequency with range of 0-100 Hz, followed by the respective exercise program35. Later, the subjects performed the warm up for the period of 10 minutes, followed by the respective interventional program for a period of 20 minutes and followed by the cool down exercises for 10 minutes. The exercises which were performed for the warm up and cool down program were: Marching in place, Calf stretching, Hamstring stretching and Illiotibial band stretch.
Figure 1: Flow diagram showing the process used in the study
Group A: Otago Exercise Program Group (OEP Group):
The subjects in this group received OEP training, 3 days in a week for 8 weeks (total = 24 sessions), with 40 mins per session. Each session included 10 mins of warm up and 10 mins of cool down exercises. The Otago Exercise Program (OEP) is a fall prevention program which addresses the risk factors of poor balance and lower limb weakness with an individually prescribed, home based exercise program for older adults31. Otago was developed to prevent fall among older adults. It is a set of exercise program consisting leg muscle strengthening, balance retraining and walking. Before starting the intervention, the subjects were briefed, demonstrated about the procedure of the exercises and also were assured for the correct performance of the exercise like, never exercise by holding on to an object which may move and not stable, follow the correct pattern of breathing, work in a pain free range, take rest interval while doing the exercise and to report to the researcher in case of any breathlessness, dizziness or chest pain in between the sessions.
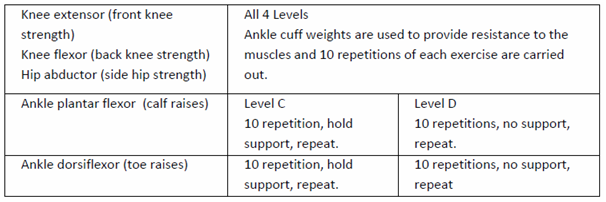
Strengthening exercises:
The strengthening exercises in the OEP group were performed with various levels from A to D. All levels were performed with ankle weights for knee flexors, knee extensors and hip abductors. Body weight was used for resistance to the ankle dorsiflexor and plantarflexor. The level C was performed with support and level D without support. The progressions were executed when patients were able to do 2 sets of ten repetitions with each exercise. The starting level resistance for the exercise for each muscle group in each leg was determined by the amount of ankle weight the patient can lift to perform 10 good quality of repetitions before fatigue.
It was started by providing 1 kg weight, it is to warm up the muscles which minimizes both muscle soreness and compliance problems, then subjects were asked to rest for 1 min time period and ½ kg weight was added to the warm up load to perform 10 repetitions without fatigue, after giving 2 min rest period, again ½ kg weight was added and the subjects were asked to perform 10 repetitions. If subject was able to perform 10 repetitions without fatigue then that weight was fixed as a resistance for the exercises, and if subject was not able to do the repetitions withoutfatigue, then after reducing the weight by 250 gm subjects were asked to continue the exercises with that weight for resistance.
The subjects were instructed to do the exercises slowly through the functional range of active joint movement with two or three seconds to lift the weight and four to five seconds to lower the weight. They were instructed to take two min rest in between the sets.
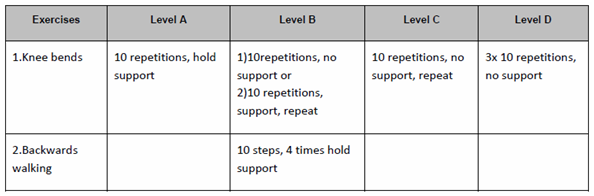
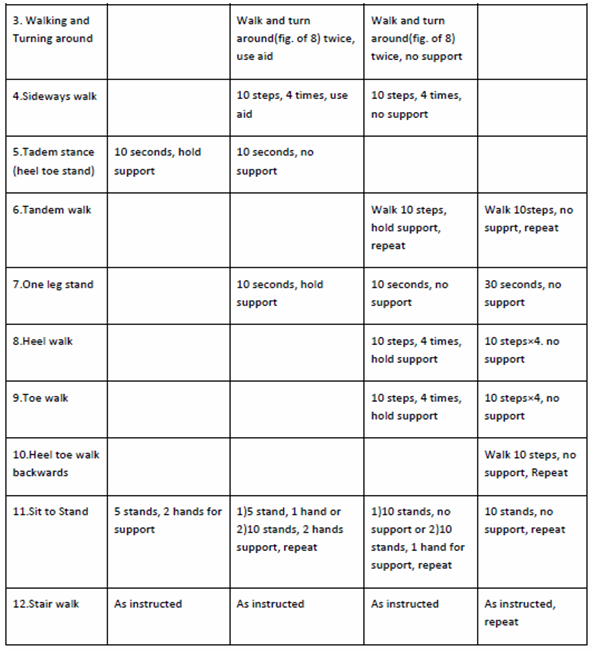
Balance re-training Exercises:
The balance exercises in the OEP were performed with levels from A to D. level A consist of knee bending exercise, tandem stance, sit to stand and stair walking exercises performed by the subjects. Level B consist of knee bending, backward walk, walking and turning around, sideways walk, tandem stance, one leg stand, sit to stand and stair walking exercises. Level C consist of knee bending, walking and turning around, sideways walk, tandem stance, one leg stand, heel walk, toe walk, sit to stand and stair walking exercises.
Level D consist of knee bending, backward walk, tandem walk, one leg stand, heel walk, toe walk, heel toe walk backwards, sit to stand and stair walking exercises. Balance exercises progress from holding on to a stable structure to performing the exercise independent of support. The subjects were made sure that they can recover their balance using lower body strategies before prescribing the exercises without support. Unstable subjects initially needed a wider base of support and all were instructed to look ahead while doing exercises. There are 12 balance exercises, with 4 levels of difficulties, which are as follows:
Walking: Subjects were asked to include walking in the exercise program to help increase physical capacity by wearing comfortable shoes and clothing. Before they start walking, warm up exercise i.e. marching on a place for two minutes should have done by the subjects. While walking subjects should look ahead, shoulders should be relaxed and arms gently swing, use walking aids if any, use prescription eyeglasses if advised, do not go outside if it is too cold or too warm, walk at a normal and not a fast pace, walk in a maintained, and well lit area. For walking, subjects should aim for up to 30 minutes, by breaking the session into shorter sessions (three 10-minute sessions), walking at their usual pace, at least twice a week. The walking should only incorporate walking plan when they are physically ready and able. They should begin walking indoors and progress to walking outdoors when strength and balance have improved.
Group B: Strength Training Program Group (STP): The subjects in this group received STP, 3 days in a week for 8 weeks (total = 24 sessions), with 40 minutes per session. Each session included 10 minutes of warm up, 20 minutes of strengthening program, and 10 minutes of cool down exercises. Strength Training program focused on strengthening the lower limb muscle groups i.e. hip flexors, hip extensors, hip abductors, knee flexors and knee extensors with the help of theraband in a color with which a subject could perform 3 sets of 10 repetitions while selected for training.
Initially the exercises were performed without resistance to make subjects comfortable. Before starting the exercise protocol, the resistance level was determined by giving yellow band to all of the subjects and they were instructed to perform 3 sets of 10 repetitions along with the rest intervals in between the sets, for 3 minutes. If subject was able to comfortably complete the repetitions, progression was done by changing the next color band i.e. red color band. If subject was not able to complete the repetitions, then resistance for strengthening was decided by returning to the previous level.
The secure anchoring of theraband was assured to a steady object before starting the exercises and subjects were asked to perform all exercises in a slow and controlled manner. They were instructed to perform all the exercises by maintaining the normal spinal curves, and not to lock the joints, or avoid hyper-extending and over flexing them. All subjects were instructed to work in a pain free range, to take the rest interval while doing the exercise and to follow the correct pattern of breathing. They were also instructed to report to the researcher in case of any breathlessness, dizziness, and chest pain in between the sessions.
Selection criteria:
Inclusion criteria: The inclusion criteria for this study were as follows:
Both male and female participants with age group between 60-69 years, Bilateral knee osteoarthritis, Complain of knee pain3, Complain of less than 30 minutes of morning knee joint stiffness3, Crepitus on active movements in knee joint3,Complain of bony tenderness around knee joint line3, TUG score of 14 sec and above27.
Exclusion criteria: Subjects were excluded if they had21, 24, 25: Any history of surgery around the knee, history of injury around the knee, deformity, neuromuscular disorders, and cardiovascular disorders.
Outcome measurements: The outcome measures used for this study were Time up and go test and 30-Sec chair stand test.
The Time up and Go test (TUG): In this study the risk of fall in bilateral knee osteoarthritis were assessed with TUG test. Here the patients were made to sit on the standard armchair with seat height of 18 inc16. The chair was having adequate back rest and positioned in such way that it didn’t move when the subject is performing the test.
The subject was asked to stand from the chair on the word “go” and walk at comfortable speed to the line marked on the floor 3 meters away from the chair then, turn around and return to sit on the chair. The subjects were timed from the word “go” until they return back to the sitting position. The data was recorded in seconds by using stopwatch. The older adults who take longer than 14 seconds to complete the TUG test have a high risk for fall16.
30-sec Chair Stand Test: Lower limb strength was tested with the 30 second chair stand test, which has been found to be a reliable and valid test, with a moderate correlation to weight adjusted 1 repetition maximum leg-press strength17. The subjects were asked to sit in a chair with seat height of 17 inc17, without armrest. The arms of the subjects were crossed at the wrist and held against the chest during the test. The subjects were asked to perform the test after the word “go” by standing up straight and sitting down on the chair as many times as possible in 30 seconds . The data was recorded until the subjects complete the number of stands in 30 seconds. At the end of 30 seconds if a participant was more than halfway up, the stand was counted. A score of 0 was awarded if any form of hand support was used. The test was stopped if any loss of balance occurred.
Variables: The variables used in the study were:
Dependent variables:
Risk of fall
Leg strength
Independent variables:
Otago exercise program (OEP)
Strength training program (STP)
Materials Used: Following materials were used for the recording purpose:
Measuring tape.
Stop watch.
Chair with straight back without arm rest.
Chair with straight back with arm rest.
Weight cuffs.
Thera band.
RESULT
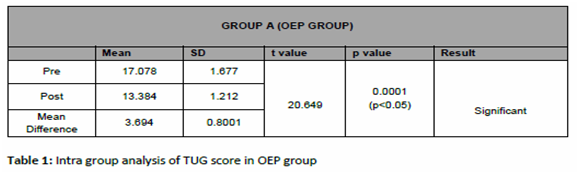
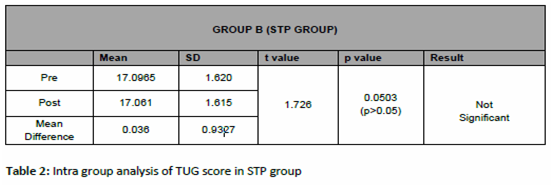
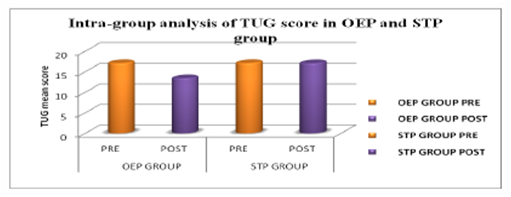
The significance of outcome measure with time up go test (TUG) on the risk of fall among bilateral knee osteoarthritis in OEP group is reflected in table 1, with p value of 0.0001 which is less than 0.05 (i.e. p<0.05) showing statistically significant results in improving the post intervention measurement score of TUG test. The significance of outcome measure with time up go test (TUG) on the risk of fall among bilateral knee osteoarthritis in STP group is reflected in table 2 ,p value of 0.0503 which is more than 0.05 (i.e. p>0.05) showing no statistical significant results in improving the post intervention measurement score of TUG test.
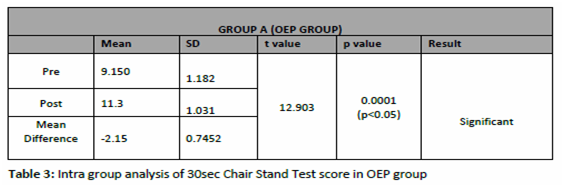
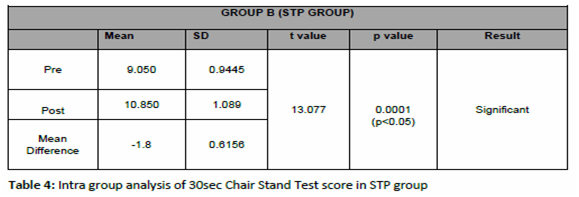
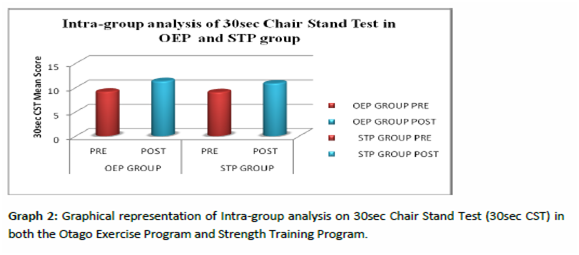
The significance of outcome measure with 30 second chair stand test (30sec CST) on the Lower limb strength among bilateral knee osteoarthritis in OEP group is reflected in table 3, which is less than 0.05 (i.e. p<0.05) showing statistically significant results in improving the post intervention measurement score of 30sec CST. And table 4 reflects the outcome measure with 30 second chair stand test (30sec CST) on the Lower limb strength among bilateral knee osteoarthritis in STP group with value less than 0.05 (i.e. p<0.05) showing statistically significant results in improving the post intervention measurement score of 30sec CST.
The significance of outcome measure of Inter-group analysis of Pre-intervention score with time up go test (TUG) in OEP group is 17.078 and STP group is 17.0965 with t value of 0.03644 and p value of 0.4856, which shows no significant results (p>0.05). The result shows that there is no discrimination in the pre scores of TUG test between both the groups. And the outcome measure with 30sec Chair Stand Test (30sec CST) on the Lower limb strength with pre-intervention mean score of OEP group is 9.15 and STP group is 9.05 with t value of 0.2956 and p value of 0.3846, which shows no significant results (p>0.05). The result shows that there is no discrimination and significant improvement in the pre test scores of 30sec CST between both the groups.
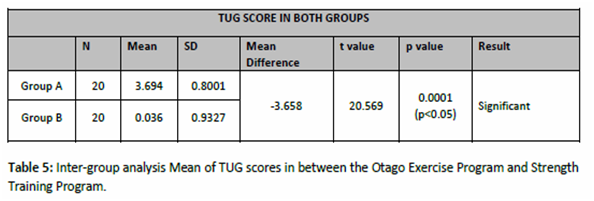
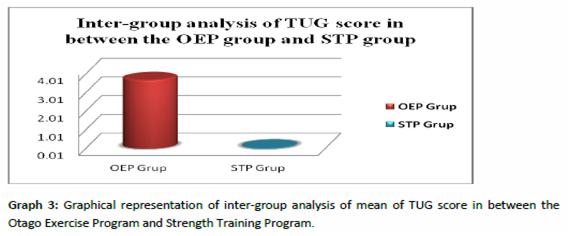
The significance of outcome measure of Inter-group analysis of mean score of time up go test (TUG) in between Otago Exercise Program and Strength Training Program group is reflected in table 5 which shows t value of 20.569 (p < 0.05) with statistical significant improvement when compared in between the two groups i.e. OEP group and STP group.
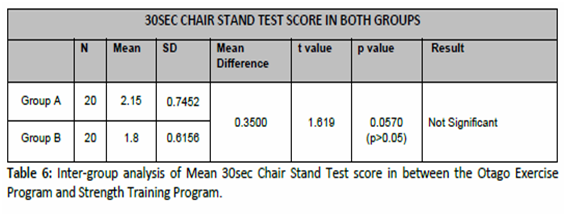
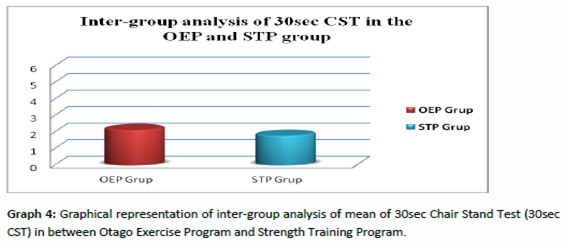
The significance of outcome measure of Inter-group analysis with mean score of 30sec Chair Stand Test (30sec CST) in between Otago Exercise Program and Strength Training Program group is reflected in table 6 which shows t value of 1.619 ( p>0.05) with no statistical significant improvement when compared in between the two groups i.e. OEP group and STP group.
DISCUSSION
The purpose of this study was to determine the effect of Otago exercise program (OEP) on risk of fall and leg strength, and to compare these effects with Strength Training Program (STP) among patients with bilateral knee osteoarthritis. In OEP group ( Group A) the results showed that there was statistically significant improvement on the risk of fall with TUG test and leg strength with 30sec Chair Stand Test in OEP (group A). On the other side the subjects in the STP (group B) showed statistical significant improvement on lower leg strength with 30sec chair stand test, but there was no statistical significance demonstrated on risk of fall with TUG. And on comparison between the groups there is statistical significant difference on risk of fall with TUG score, whereas there is no statistical significant difference with 30sec chair stand test for lower leg strength.
Thus, it showed that the OEP is effective in improving both the outcome measures, than on STP which showed improvement only on lower leg strength.The results is supported by Province et.al.21 that exercises including balance retraining reduces risk of fall in older adults. Similarly it is stated that morelimitation in functional ability in subjects with poor proprioception26, which is observed in patients with knee OA, where there is articular damage reducing the quadriceps motorneuron excitability leading to decrease in voluntary quadriceps activation. Thus, contributing to quadriceps weakness and diminished proprioceptive acuity. This arthrogenic impairment in quadriceps sensorymotor function and decreased postural stability is proved to be associated with reduced functional performance of the patients36. Also the physical function improves contributing to an effective reduction in fall among elderly people on strength and balance training29.
In addition, strengthening exercises using body weight have demonstrated a decrease in accidental fall9. The training in the OEP group of this study improves the functional ability which results in improved balance. And on the other outcome measure with 30sec CST in OEP group the results showed significant results in improving 30sec CST score indicating that there is improvement in leg muscle strength, which is important to perform day to day activities, transferring, walking, etc. in elderly bilateral knee osteoarthritis patients. The exercises which were included in the OEP, helped to improve the strength of the leg musculature in and around the knee joint reflecting on the 30sec CST, supported by Joshua N. Farr (2010)23, that patients with osteoarthritis of the knee, improved muscle strength when engaged into structured resistance exercise program. And exercises using body weight as a resistance with sufficient intensity improves the strength in the lower limb9.
The STP (group B) showed with no statistical significant improvement on TUG but it showed statistically significant improvement on 30sec CST, this result showed that there is improvement in functional leg strength but not on risk of fall which reflected on TUG. The result of this study is supported by Moreland JD et.al.(2003)30, the strength training alone is not effective in reducing the risk of fall in older adults. This result could be due to the effect of strengthening exercises, which is mainly on improving the strength of leg musculature than on improving balance, which is the most important reason to reduce risk of fall in older adults with bilateral knee osteoarthritis. As stated by Julie M Chandler (1997)22 the lower extremity strength gain with the help of strengthening exercises is associated with gains in chair rise performance, gait speed, and in mobility tasks, but not with improved balance, endurance, or disability. It is likely that impaired balance is a stronger risk factor for fall than poor muscle strength. Some studies have found the similar results that the strength training is more effective in improving the leg strength than improving balance in elderly people31,32. Similar results observed by Foley et.al.(2003)33,28 showed that the 8 of strength exercises on individual with lower extremity osteoarthritis improves strength, walking distance and physical function. Robert Topp et.al. (2002)18 also found that the resistance training improves the strength and functional ability of patients with bilateral knee OA.
In addition to the above reason, inclusion of walking in the exercise program, also showed improvement in results, and other studies have shown that walking programs have health benefits including improved fitness, weight loss, and lower blood pressure34. With appropriate prescription and supervision, exercise that challenges balance can be administered safely in the elderly population.
For example, it has been demonstrated that the Otago Exercise Program is feasible and safe for older people to undertake at home and have produced 35% reduction in fall and fall-related injury37.
Hence, the present study provides strong evidence that Otago exercise program has its effect both in reducing the risk of fall and increasing the leg strength in older adults with bilateral osteoarthritis of knee than compared with Strength Training Programme group.
CONCLUSION
This present study provides promising results in reducing risk of fall and improving leg strength with the help of Otago Exercise Program which is the combination of strength training, balance retraining and walking program, as compared with the Strength training Program in the older adults with bilateral knee osteoarthritis. So on the basis of the present study, it can be concluded that the Otago Exercise Program is effective in improving the leg strength and reducing the risk of fall, and can be used in the exercise program of older adults with bilateral osteoarthritis of knee.
REFERENCES
- Felson DT, Lawrence RC, et al. (2000). Osteoarthritis: new insights. Part 1: the disease and its risk factors. Ann Intern Med.. 8;133,635-646.
- Wolf AD, Pfleger B, et.al. (2003). Burden of Major Musculoskeletal Conditions. Policy and Practice. Special Theme-Bone and Joint Decade 2000-2010. Bulletin of the World Health Organization. 81;9, 646-656.
- R. Altman, E. Asch, et al. (1986). The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the knee. Arthritis Rheum. 29:1039–1049.
- Benjuya N, Melzer, I, et.al. (2004). Aging-induced shifts from a reliance on sensory input to muscle co-contraction during balanced standing. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 59; 2, M166.
- Tibor Hortoba, et. al. (2004). Aberrations in the Control of Quadriceps. Arthritis Care & Research. 51; 4, 562–569.
- Fitzpatrick R, Mc Closkey D., et.al. (1994). Proprioceptive, visual and vestibular thresholds for the perception of sway during standing in humans. Journal of Physiotherapy. 478;1, 173-86.
- Lord S R, Lloyd D G, et.al. (1996). Sensori-motor function, gait patterns and fall in community-dwelling women. Age Ageing. 25, 292-9.
- Schot, Knutzen, Poole, et.al. (2003). Sit-to-Stand Performance of Older Adults following Strength Training Research Quarterly for Exercise and Sport. 74;1
- Lord S, Ward JA, et.al. (1995). The effect of a 12-month exercise trial on balance, strength, and fall in older women: a randomised controlled trial. Journal of the American Geriatrics Society, 43;1198-1206.
- Campbell A.J, Borrie M.J, et.al. (2010). Circumstances and consequences of fall experienced by a community population 70 years and over during a prospective study. Age and Ageing, 19;2,136-141.
- Yusuke Maeda et al. (2011). A Preliminary study of static and dynamic standing balance and risk of falling in an independent elderly population with a particular focus on the limit of stability test. J.Physical.Therapy.Science. 23;803-806.
- Odenheimer G, Funkenstein HH, et.al. (1994). Comparison of neurologic changes in ‘successfully aging’ persons vs. the total aging population. Archives of neurology. 51;573-580.
- Perta von Heideken Wagert, Yngve Gustafson, et.al. (2009). Large variations in walking, standing up from a chair, and balance in women and men over 85 years: an observational study. Australian Journal of Physiotherapy; 55;39-45.
- Wolfson C. Wentzel, et.al. (2001). Progression of impairment in patients with vascular cognitive impairment without dementia. Journal of Neurology. 28, 57;4, 714-716.
- Podsiadlo D, Richardson S, et.al. (1991).The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 39;142–148.
- Shumway-Cook A, Brauer S, et.al. (2000). Predicting the probability for fall in community-dwelling older adults using the Timed Up & Go Test. Phys Therapy. 80;896 –903.
- Jones CJ, Rikli RE, et.al. (1999). A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. J Am Geriatric Soc. 70;2,113-9.
- Robertson, Campbell, Gardner, et.al. (2002). Preventing Injuries in Older People by Preventing Fall: A Meta-Analysis of Individual-Level Data Journal of the American Geriatrics Society. 50;5, 905-911.
- Rubenstein LZ, Josephson KR, et.al. (2002).The epidemiology of fall and syncope. In: Kenny RA, O’Shea D, eds. Fall and Syncope in Elderly Patients Clinics in Geriatric Medicine. Philadelphia: W. B. Saunders Co. 28, 513-518.
- M. Province, Evan C. Hadley et al.(1995). The Effects of Exercise on Fall in Elderly PatientsA Preplanned Meta-analysis of the FICSIT Trials. JAMA. 273;17,1341-1347.
- Campbell AJ, Robertson MC, Norton RN, et.al. (1999).Fall prevention over 2 years: a randomized controlled trial in women 80 years and older. Age and Ageing. 28,513-518.
- Julie M. Chandler, Pamela W. Duncan, et.al. (1998). Is lower extremity strength gain associated with improvement in physical performance and disability in frail, community-dwelling elders. American Congress Of Rehabilitation Medicine And The American Academy Of Physical Medicine And Rehabilitation. 003-9993/98/7901-4303.
- Joshua N. Farr, Scott B. Going, et.al. (2010). Progressive Resistance Training Improves Overall Physical Activity Levels in Patients With Early Osteoarthritis of the Knee: A Randomized Controlled Trial. J Physical Therapy. 90:356-366.
- Cathy M Arnold, Robert A. Faulkner, et.al. (2010). The Effect of Aquatic Exercise and Education on Lowering Fall Risk in Older Adults With Hip Osteoarthritis Journal of Aging and Physical Activity, 18;245-260.
- Marie-Louise Bird, Keith Hill, et.al. (2009). Effects of Resistance- and Flexibility-Exercise Interventions on Balance and Related Measures in Older Adults. Journal of Aging and Physical Activity, 17;444-454.
- M. Van der esch, M. Steultjens, et.al. (2007). Joint proprioception, muscle strength, and functional ability in patients with osteoarthritis of the knee. American college of rheumatology. 57,5,787–793.
- Julie C. Whitney, Stephen R. Lord, et.al. (2005). Streamlining assessment and intervention in a fall clinic using the Timed Up and Go Test and Physiological Profile Assessments. Age and Ageing. 34;567–571.
- Robert Topp, Sandra Woolley, et.al. (2002). The effect of dynamic versus isometric resistance training on pain and functioning among adults with osteoarthritis of the knee. American Congress of Rehabilitation Medicine and the American Academy of Physical Medicine and Rehabilitation. 83;1187-95.
- Campbell, A.J., Borrie, M.J., et.al. (1990). Circumstances and consequences of fall experienced by a community population 70 years and over during a prospective study. Age and Ageing. 19;2,136-141.
- Moreland JD, Richardson JA, et.al. (2004). Muscle weakness and fall in older adults: a systematic review and meta-analysis. Journal of the American Geriatrics Society. 52,1121-1129.
- Orr R, Raymond J, Fiatarone Singh M, et.al. (2008). Efficacy of progressive resistance training on balance performance in older adults: A systematic review of randomized controlled trials. Sports Med 38;317-343.
- Latham N, Anderson C, Bennett D et al. (2003). Progressive resistance strength training for physical disability in older people. Cochrane Database Syst Rev. The Gerontolo Society of America. 2;33-36.
- 33. Foley A, Halbert J, et.al. (2003). Does hydrotherapy improve strength and physical function in patients with osteoarthritis: a randomised controlled trial comparing a gym based and a hydrotherapy based strengthening programme. Ann Rheum Dis; 62,1162–7.
- Murphy MH, Nevill AM, et al. (2007). The effect of walking on fitness, fitness and resting blood pressure: A meta-analysis of randomized, controlled trials. Prev Med 44,377-385.
- Ruth Defrin, Efrat Ariel, et.al. (2005).Segmental noxious versus innocuous electrical stimulation for chronic pain relief and the effect of fading sensation during treatment. Science, Direct., 115;1-2,152–160.
- 36. Michael V Hurley, David L Scott, et.al. (1997).Sensorimotor changes and functional performance in patients with knee osteoarthritis. Annals of the Rheumatic Diseases. 56;641-648.
- Robertson MC, Campbell AJ, Gardner MM et al. (2002). Preventing injuries in older people by preventing fall: A meta-analysis of Individual-Level Data Journal of the American Geriatrics Society. May 50;5, 905-911.
Citation:
Kanchan A. Katre, Vijayakumar Pushparaj, Jibi Paul (2019). Effect of Otago Exercise Program (OEP) and Strength Training Program (STP) on leg strength and risk of fall among bilateral knee osteoarthritis patients, ijmaes, 5(1), 536-551.

Leave a Reply