To study the relationship of neck circumference as a parameter in predicting Metabolic Syndrome- A One year cross sectional study
Dr. Bobby Varghese1, Dr. Rekha S Patil2
Co-Author:
2Dr. Rekha S Patil, MD, Professor and Head, Department of Medicine, J. N. Medical College, Nehru Nagar, Belgaum, Karnataka, India.
Corresponding Author:
1Dr. Bobby Varghese MD, Consultant Physician, Holy cross Hospital, Adoor, Kerala, India, E-mail: dr.bobbyv@gmail.com
Abstract
Background and objectives: Upper-body fat distribution has long been recognized as related to increased cardiovascular disease risk, and neck skin fold or NC has been used as an index for such an adverse risk profile. This study was aimed to evaluate the relationship of NC as a parameter in predicting metabolic syndrome.
Methodology: The present study was conducted in the Department of Medicine, KLES Dr. Prabhakar Kore Hospital and Medical Research Centre, Belgaum during the study period from January 2011 to December 2011. Hundred (100) cases of metabolic syndrome were taken based on NCEP ATP III criteria and the various components of metabolic syndrome and the NC were evaluated and compared.
Result: In this study 66% of the patients were males and 34% were females. Mean age of the study population was 54.46 ± 14.93 years. 46% of the patients had metabolic syndrome with four components and 31% had five components. The commonest component of metabolic syndrome was hypertension (95%) followed by hyper triglyceridemia (82%). Abnormal NC was observed in 97% patients and mean neck circumference was 38.93±1.95 centimeters. Waist circumference was abnormal in 74% patients. The mean waist circumference of the study population was 97.9±7.44 centimeters. Lipid abnormalities of total cholesterol, LDL, triglycerides and HDL were noted in 30%, 18%, 82% and 76% of the patients respectively.
Conclusion: Patients with metabolic syndrome presented with abnormal NC, which was not associated with any of the components of metabolic syndrome. However, elevated BMI had associated increased neck circumference and this association was statistically significant.
Keywords: Body mass index, metabolic syndrome, neck circumference (NC), upper body fat, waist circumference.
Received on 16th July 2015, Revised 28th July 2015, Accepted 18th Aug 2015
INTRODUCTION
The metabolic syndrome is a cluster of risk factors for cardiovascular disease (CVD), including obesity, hypertension, elevated triglycerides and low levels of HDL Cholesterol. The clinical manifestations of this syndrome include hypertension, hyperglycaemia, reduced high- density lipoprotein cholesterol (HDL-C), hypertriglyceridemia and abdominal obesity.
Approximately one fourth of the adult European population is estimated to have metabolic syndrome, with a similar prevalence in Latin America.1 Metabolic syndrome is also considered as an emerging epidemic in developing East Asian countries including China, Japan, and Korea. The prevalence of metabolic syndrome may range from 8 to 13% in men and 2 to 18% in women depending on the population and definitions used.2 In Japan, the Ministry of Health, Labor, and Welfare has instituted a screening and interventional program. Metabolic syndrome has been recognized as a highly prevalent problem in many other countries worldwide.3-5
It is accepted that metabolic syndrome increases the relative risk of cardiovascular disease, though it is still debated whether metabolic syndrome adds to global cardiovascular disease risk assessed by traditional risk factors. It is believed that visceral adiposity lies at the root of the cardio metabolic risk with the consequent syndrome of central obesity/insulin resistance. Clinical definitions of metabolic syndrome by National Cholesterol Education Program-ATP-III6 or International Diabetes Federation7 have been of enormous value in the diagnosis, management and research on the cluster of metabolic risk factors. Yet, there is increasing recognition that other atherogenic, pro-thrombotic and inflammatory aspects of this syndrome are not captured by these practical clinical definitions which warrant further investigation, particularly for valuable clinical markers.8
Upper-body fat distribution has long been recognized as related to increased cardiovascular disease risk, and neck skinfold9 or neck circumference (NC) 10 has been used as an index for such an adverse risk profile. Free fatty acid release from upper-body subcutaneous fat was reported to be larger than that from lower-body subcutaneous fat.11
Although obesity results in metabolic abnormalities, upper body obesity is more strongly associated with glucose intolerance, hyperinsulinemia, uric calculus, diabetes hypertriglyceridemia and gout disease than lower body obesity. Upper body obesity can be assessed by various techniques such as NC, waist circumference (WC), waist-to-hip ratio, waist-to- thigh ratio, sub scapular-to-triceps skin fold ratio and abdominal sagittal diameter.
NC was found to be a simple and time-saving screening measure that could be used to identify overweight and obese individuals. It has been shown that men with a NC of less than 37 cm and women with a NC of less than 34 cm probably have a less chance of developing metabolic syndrome. Patients above these levels require a more comprehensive evaluation of their status as overweight or obese.12
Epidemiological population-based studies on the clinical significance of NC in regard to metabolic syndrome are lacking. Disorders in lipid or glucose metabolism and fasting hyperinsulinemia were found to prevail highest in the highest quintile of NC in a study from Finland.13
NC was proposed as a screening measure for identifying overweight and obese individuals in 979 Israeli adults visiting a family medicine clinic and sex specific optimal cut-off points were proposed. In a subset of the mentioned group, higher NC was found correlated positively with the factors of the metabolic syndrome. NC was also a good correlate of raised androgens in 107 severely obese premenopausal women.14
Objective of this study was to evaluate the relationship of neck circumference as a parameter in predicting metabolic syndrome.
METHODOLOGY
The present study was conducted in the Department of Medicine, KLES Dr. Prabhakar Kore Hospital and Medical Research Centre, Belgaum on patients with metabolic syndrome during the period of January 2011 to December 2011.
The study design was one year cross sectional study. The Study period and duration was one year conducted during the period of January 2011 to December 2011.
Data collected from the patients admitted in the wards of Medicine Department or attending the Medicine OPD/executive health check-up schemes on Mondays, Wednesdays and Fridays at KLES Dr. Prabhakar Kore Hospital and Medical Research Centre, Belgaum was studied.
Sample size: Hundred (100) patients with metabolic syndrome were selected for the study.
Sampling method: Every third patient fulfilling the inclusion criteria were included in the study.
Selection criteria
Inclusion Criteria: Age above 18 years and Patients with metabolic syndrome based on National Cholesterol Education Program-ATP-III criteria
Exclusion Criteria: Patients with spine deformities, Patients with neck swellings like goiter, Patients who have been diagnosed with turners’ syndrome, Patients who had undergone surgeries in neck, Patients with cervical lymphadenopathies, surgical emphysema in the neck and cellulitis of neck.
National Cholesterol Education Program-ATP-III criteria for metabolic syndrome
Three or more of the following:
- Abdominal obesity (waist circumference
> 102 cm in men, >88 cm in women)
- Triglycerides ≥ 150 mg/dL.
- HDL-cholesterol < 40 mg/dL in men, < 50 mg/dL in women.
- Systolic blood pressure ≥130 mmHg and/or diastolic blood pressure ≥85 mm Hg.
- Fasting plasma glucose ≥ 110 mg/dL.
Ethical clearance
The study was approved by the Institutional Ethics Committee of Jawaharlal Nehru Medical College, Belgaum.
Informed consent
Patients admitted in the wards of Medicine Department or attending the Medicine OPD/executive health check-up schemes on Mondays, Wednesdays and Fridays at KLES Dr. Prabhakar Kore Hospital and Medical Research Centre, Belgaum were evaluated based on selection criteria. The selected patients were briefed about the nature of the study and a written informed consent was obtained.
Data collection
Demographic data like gender and age were collected along with relevant history and recorded on predesigned and pretested proforma (Annexure-II). A thorough clinical examination was conducted and the findings were also recorded. Body mass index was calculated based on formula;
Body mass index was calculated based on formula;
Body mass index in the range of less than 18.5 kg/m2 were considered as underweight, 18.5 to 24.9 kg/m2 were considered as normal, 25.0 to 29.9 kg/m2 were considered as overweight and more than 30 kg/m2 were considered as obese.15
The waist circumference was measured using a standard measuring tape in cms. Waist circumference of > 102 cms in males and > 88 cms in females was considered abnormal.
Neck circumference was measured to the nearest 0.1 centimeter just below the laryngeal prominence (Adam’s apple) perpendicular to the long axis of neck in both sexes with the subjects standing upright, with shoulders relaxed using flexible measuring tapes. Neck circumference of ≥ 37 cms in males and ≥ 34 cms in females was considered abnormal.
Blood pressure was recorded in the sitting position after five minutes of rest using standard mercury manometer. Three readings were taken at an interval of one minute and mean BP was calculated.
Fasting blood samples were drawn for investigations such as FBS and lipid profile (total cholesterol, triglycerides, HDL and LDL)
Statistical analysis
The data obtained was tabulated on Microsoft Excel spreadsheet. Categorical data was expressed as rates, ratios and percentages. Fisher exact test was used to assess the level of significance between NC and components of metabolic syndrome. Continuous data was expressed as mean ± standard deviation (SD) and the comparison was done using student unpaired ‘t’ test. Correlation coefficient (r) was used to assess the correlation between NC and components of metabolic syndrome. SPSS 18 trial version software was used for analysis. A probability value (‘p’ value) of less than or equal to 0.050 was considered as statistically significant.
RESULT
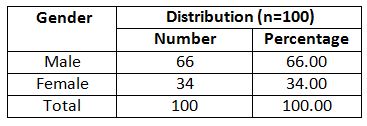
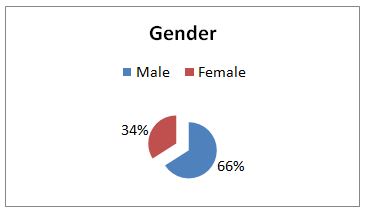
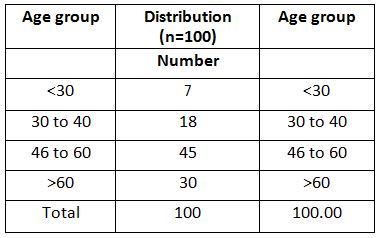
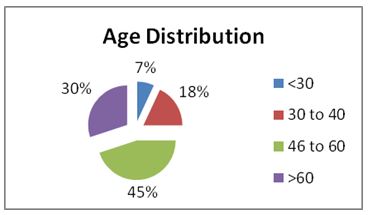
This study involved both male and female group of population, male with 66% and female with 34% (Table 1)
Age Distribution: The table 2 shows the distribution of subjects according to age. The mean age for the study population was 54.46 ± 14.93 years.
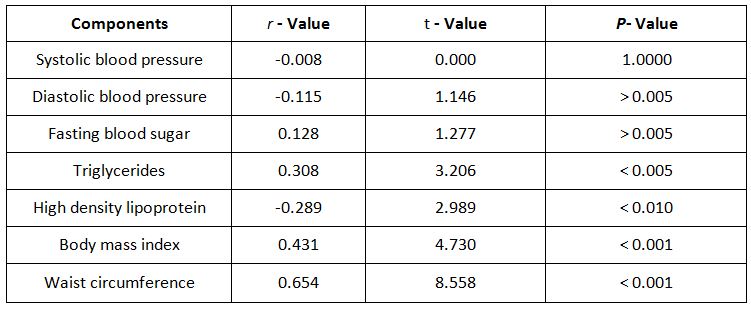
Relationship of neck circumference with other parameters
The study analysed the correlation co-efficient between neck circumference and components of metabolic syndrome. There was statistically significant correlation found between neck circumference and metabolic components such as triglycerides, high density lipoprotein, body mass index and waist circumference, whereas no correlation was found between neck circumference and components like blood pressure (systolic and diastolic) and fasting blood sugar (Table 3).
DISCUSSION
Measurement of NC has recently been used to identify overweight and obesity and is observed to have good correlation with age, weight, waist and hip circumferences, waist-to-hip ratio, and BMI for both genders. Besides, NC is considered an index of upper body obesity and correlates positively with changes in systolic and diastolic blood pressure and other components of the metabolic syndrome. NC measurements are an alternative and innovative approach for determining body fat distribution.16
Neck circumference as an index for upper-body subcutaneous adipose tissue distribution has been evaluated in relation to cardiovascular risk factors, insulin resistance, and biochemical components of metabolic syndrome.17 However, studies on role of NC in predicting the metabolic syndrome are scarce and so far there are no Indian studies available. Hence the present study was undertaken to evaluate the relationship of NC as a parameter in predicting metabolic syndrome.
The present study was conducted in the Department of Medicine, KLES Dr. Prabhakar Kore Hospital and Medical Research Centre, Belgaum during the study period from January 2011 to December 2011. Hundred (100) cases of metabolic syndrome (based on NCEP ATP III criteria) were taken and the various components of metabolic syndrome and the NC were evaluated and compared. The NC was measured at a level just below the laryngeal prominence perpendicular to the long axis of neck. This is in sharp contrast with one study done in Andhra Pradesh which showed metabolic syndrome rates were significantly higher among females. Females accounted for 52.2% (n=307) whereas males were only 34.2% (n=202). 18
This difference could be because of number of males and females patients studied (total of 509). Majority of the subjects were between 46 to 60 years accounting for 45%, with 30 subjects in the age group > 60. Overall, the mean age for the study population was 54.46 ± 14.93 years. In an Indian study, significantly higher rates of metabolic syndrome were observed in older age groups. The incidence of metabolic syndrome increased with increasing age in such a way that the incidence was around 6% in the age group of 20 -29 years peaking to around 65 % in the age group of 60-69 years. 19
In this study past history of diabetes was present in 63 patients and hypertension in 80 patients. Three patients reported a history of cerebrovascular accident and 10 patients had ischaemic heart disease. Of the 63 diabetic patients, 33 of them had diabetic retinopathy and only 2 had diabetic nephropathy. History suggestive of peripheral vascular disease and peripheral neuropathy was found in one patient each.
A study of metabolic syndrome in Asian Indians, all the individual components of metabolic syndrome increased significantly with age. Elevated blood pressure (63.1%) was the commonest abnormality observed. 20
In a study done in the University of Oslo, among patients with metabolic syndrome, 29% had diabetes. On the other hand, in a prevalence study of metabolic syndrome and its components in urban India, diabetes was found in 82.01% of patients. 21
An Indian study have shown that Diabetes and Hypertension are found more widely prevalent in South Asians, thus conferring a large and very real risk of adverse cardiovascular events and other attending complications. The possible explanations for this inordinately high prevalence can be attributed to a high prevalence of obesity, insulin resistance and a body fat structure that favours the development of metabolic syndrome, Diabetes and Hypertension.22
In the present study, 66% of the patients were in the overweight group (BMI between 25 to 29.99 kg/m2) and 18% of the patients were obese (BMI of > 30 kg/m2). However, 16% patients had a normal BMI (between 18.5-24.99 kg/m2). Overall the mean BMI of the study population was 27.8 ± 2.99 Kg/m2.
In a study done in Norway, the mean BMI in patients with metabolic syndrome was found to be 28.4 kg/m2 (26.6-30.6)23. In the National health statistics report of 2009, 29.8% of subjects were overweight and 65% of subjects were obese. In a study of urban Indian population, they found that 79.01% of the subjects had a BMI of > 24.9 Kg/m2.
An Indian study showed that metabolic syndrome and cardiovascular risk in Asian Indians/South Asians are heightened by their relative increase in body fat mass, truncal subcutaneous fat mass, intra-abdominal fat mass, and also by ectopic fat deposition. South Asians also seem to have a peculiar body phenotype known as South Asian Phenotype, characterized by increased waist circumference, increased waist hip ratio and excessive body fat mass. 24
In this study, 74% of the patients had abnormal waist circumference whereas in 26% waist circumference was within the normal range. Overall, the mean waist circumference for the study population was found to be 97.9 ± 7.44 cms. Among males the mean waist circumference was 101.30 ± 6.18 cms and in females it was 91.18 ± 4.60 cms.
Another study done in Taiwan according to the National Cholesterol Education Program Adult Treatment Panel III criteria, waist circumference abnormality was seen in 40% in 11411 adults. 25
A study done in China showed that waist circumference (WC) and body mass index (BMI) were good markers for MetS. WC was a good marker for T2 DM and dyslipidemia, and BMI was a good marker for hypertension. The optimal BMI cut-off value of MetS was 24 kg/m², and the optimal WC cut-offs were 86 cm and 78 cm in men and women, respectively. 26
In the present study 97% of the patients had abnormal neck circumference. Overall, the mean neck circumference was 38.93±1.95 cms. Among the males the mean neck circumference was 39.83 ± 1.68 cms and in females it was 37.17 ± 1.00 cms.
In a similar study done in the Istanbul University, Istanbul, Turkey, the mean NC measured among patients with metabolic syndrome was 36.7 cm in the total sample. With a mean of 38.8 cm in men, it was 4 cm wider than in women (34.8 cm). 27
In this study, overall 95 (95%) patients had hypertension of which, 80 (80%) were known hypertensive and 15 (15%) were newly detected. However, in 5% normal blood pressure was recorded.
In the present study 81% of patients were diabetics. Among these, 63 (63%) patients were known diabetics and 18 (18%) were detected with abnormal FBS. However, 19% patients had normal FBS levels.
In this study, the lipid profile revealed majority of the patients with abnormal triglycerides (82%) and HDL (76%) levels whereas elevated total cholesterol levels were noted in 30% of patients. Abnormal LDL was noted in only 18% of the patients.
In another study146 done in New Delhi, India, the age-adjusted HDL levels were found to be low in 64.91% of subjects.
In a study done on Asian-Indians (Chennai), abnormal TG and HDL levels were seen in 76% and >90% of the study population. Asian Indians were found not only to have low HDL, but also have a preponderance of small, dense, dysfunctional HDL particles that are associated with less efficient reverse cholesterol transport and less protection against CAD.138 In a sub-study of the Chennai rural epidemiology study, abnormal Triglycerides and HDL were found in 25.2% and 63.5% of the patients respectively. However, in a study done only on urban south Indian men, abnormal TG was seen in 45.2%, whereas abnormal HDL was seen in 70.3% of subjects. 28
In the present study the most common component of metabolic syndrome was hypertension 95%, followed by hypertriglyceridemia 82%, elevated fasting blood sugar 81%, low HDL 76% and abnormal waist circumference 74%.
In the present study 46% patients
had metabolic syndrome with four components and 31% had five components.
However 23% of the patients were noted with three components of metabolic
syndrome. In patients with 3 components of metabolic syndrome (n=23), abnormal
NC was found in 21 patients (91.3%) whereas 2 patients (8.7%) had normal neck
circumference. In patients with 4 components of metabolic syndrome (n=46),
abnormal NC was found in 45 patients (97.83%) whereas one patient (2.17%) had
normal neck circumference. All the patients with five components of metabolic
syndrome (n=31), had abnormal NC.
In this study the mean neck circumference among patients with five components was slightly higher (39.73 ± 2.25) compared to patients with three (38.42 ± 1.33) and four (38.64 ± 1.85) but, this difference was statistically not significant.
In the present study, among all the overweight (BMI 25.00 to 29.99 Kg/m2) and obese (BMI > 30.00 Kg/m2) patients the NC was abnormal (100%) and this difference was statistically significant (p=0.003). The mean neck circumference among normal, overweight and obese showed an increasing trend (37.27 ± 1.98, 38.91 ± 1.53 and 40.45 ± 2.15 respectively).
In this study among the 74 patients with abnormal waist circumference NC was abnormal in 98.65% and normal in 1.35% suggesting most of the patients with abnormal waist circumference had elevated NC. The mean NC in patients with normal and abnormal waist circumference was 38.53 ± 1.37 and 39.06 ± 2.1 respectively. However these findings were statistically not significant.
In the present study, of the 95 patients with hypertension, NC was elevated in 96.84% which was not statistically significant. The mean NC did not vary significantly in normotensive and hypertensive patients.
In the RENATA study done in Argentina hypertension was found in 57.4% of the patients with abdominal and neck obesity.29In our study, of the 81 patients with abnormal FBS, 79 (97.53%) had elevated NC but this difference was not statistically significant. The mean NC did not vary significantly among normoglycemics and hyperglycemics.
In the present study, of the 82 patients with hypertriglyceridemia, 97.56% had elevated NC. The mean NC in patients with hypertriglyceridemia was 39.14 ± 1.98 and in those with normal triglyceride levels it was 37.97 ± 1.46 cms. However these differences were statistically not significant.
In our study among the 76
patients with abnormal HDL levels, NC was elevated in 97.37% patients but no
statistically significant association was
found between abnormal HDL and NC.
The mean NC levels were 38.7 ± 1.74 cms and 39.0 ± 2.01 cms in patients with
normal and abnormal HDL levels respectively.
In this study statistically significant correlation was found between neck circumference and metabolic components such as triglycerides, high density lipoprotein, body mass index and waist circumference whereas no correlation was found between neck circumference and components like blood pressure (systolic and diastolic) and fasting blood sugar.
In a similar study done in the Istanbul University, Turkey, correlation coefficients were high between NC and waist hip ratio, but were particularly high with waist circumference and BMI, exhibiting r value of 0.6 or over. 30
Another study done in Israel indicated a strong correlation between NC and BMI (total adiposity index), as well as between NC and WC and waist- to-hip ratio (upper-body obesity indexes). NC was also strongly correlated with SBP, DBP, total cholesterol, LDL-cholesterol, triglycerides, fasting glucose, and uric acid levels. No significant correlation was found between NC and HDL- cholesterol levels. 31
This difference in our study and other studies may be because of number of patients in the study group. As a main finding in this cross-sectional analysis of data among patients with metabolic syndrome, we found NC as an indicator of central obesity and metabolic syndrome. This novel finding presumably reflects fat deposition in an ectopic site, such as observed in fatty liver or in the thoracic visceral adipose tissue that may include (basal areas of) the neck and palate.
A study in 166 patients with and without Mets demonstrated a clear relationship between epicardial fat, assessed by echocardiography and activity of hepatic serum alanine and aspartate aminotransferases in subjects with increased visceral adiposity, an association which seemed to be independent of BMI.32
Furthermore, threshold values of echocardiographic epicardial fat measurements were proposed for men and women, which could be of help for cardio-metabolic risk stratification. Newly, evidence was provided that peri-coronary epicardial adipose tissue was associated with CT- assessed coronary artery calcification in 573 healthy post-menopausal women suggesting the possibility that local fat may drive the development of atherosclerosis.
Limitations of the study
The present study’s cross-sectional nature limits to some extent its interpretation as to causality of associations. Evaluation of NC based on single measurements might be considered a minor limitation.
Conclusions reached may not be fully applicable to a population because of the relative small sample size of the present study. Further studies with larger sample sizes are needed to identify the relationship of NC with central obesity and MS in general population.
CONCLUSION
In this study majority of the patients with metabolic syndrome presented with abnormal NC. But, abnormal neck circumference was not associated with any of the components of metabolic syndrome. Patients with elevated BMI had associated increased neck circumference and this association was statistically significant. Correlation test revealed that neck circumference was significantly correlating with triglycerides, high density lipoprotein and waist circumference. However, no correlation was seen between neck circumference and blood pressure (both systolic and diastolic) and fasting blood sugar.
REFERENCES
- Grundy SM. Metabolic syndrome pandemic. Arterioscler Thromb Vasc Biol 2008; 28(4):629- 36.
- Hoang KC, Le TV, Wong ND. The metabolic syndrome in East Asians. J Cardiometab Syndr 2007; 2(4):276-82.
- Hwang LC, et al. Prevalence of obesity and metabolic syndrome in Taiwan. J Formos Med Assoc 2006; 105(8):626-35.
- Kolovou GD,et al. The prevalence of metabolic syndrome in various populations. Am J Med Sci 2007; 333(6):362-71.
- Kaaja R, et al. The increasing prevalence of metabolic syndrome among Finnish men and women over a decade. J Clin Endocrinol Metab. 2008; 93(3):832-6.
- Ersoz HO, et al. Prevalence of metabolic syndrome and associated risk factors among Turkish adults: Trabzon MetS study. Endocrine. 2008; 33(1):9-20.
- Gupta VP, et al. Persistent high prevalence of cardiovascular risk factors in the urban middle class in India: Jaipur Heart Watch-5. J Assoc Physicians India. 2012;60:11-6.
- Alberti KG, Zimmet P, Shaw J. The metabolic syndrome – a new world-wide definition. Lancet 2005; 366:1059–62.
- Despre´ s J-P, et al. From individual risk factors and the metabolic syndrome to global cardiometabolic risk. Eur Heart J Suppl 2008; 10(Suppl. B):B24–133.
- Vague J. The degree of masculine differentiation of obesities:a factor determining predisposition to diabetes, atherosclerosis, gout, and uric calculous disease. Am J Clin Nutr 1956; 4:20–34.
- Hakangard AC, et al. Body compartment and subcutaneous adipose tissue distribution – risk factor patterns in obese subjects. Obes Res 1995; 3:9–22.
- Lissner L, et al. Relationship between changes in body composition and changes in cardiovascular risk factors: the SOS intervention study: Swedish obese subjects. Obes Res 1997; 5:519–30.
- Laakso M, et al. Association of neck circumference with insulin-related factors. Int J Obes 2002; 26:873–5.
- Ben-Noun L, Sohar E, Laor A. Neck circumference as a simple screening measure for identifying overweight and obese patients. Obes Res 2001;9:470–7.
- Ben-Noun L, Laor A. Relationship of neck circumference to cardiovascular risk factors. Obes Res 2003; 11:226–31.
- Dixon JB, O’Brien PE. Neck circumference as a good predictor of raised insulin and free androgen index in obese premenopausal women:changes with weight loss. Clin Endocrinol 2002; 57:769–78.
- Wang SY, et al. Prevalence and determinants of prehypertension status in the Taiwanese general population. J Hypertens 2005; 23: 1355-60.
- Grotto I, et al. Prevalence of prehypertension and associated cardiovascular risk profiles among young Israeli adults. Hypertension 2006; 48: 254-9.
- Ryu OH, et al. Prevalence of prehypertension and hypertension in a Korean population: Korean National Health and Nutrition Survey 2001. J Hypertens 2006; 24: 1515-21.
- Hingorjo MR, Qureshi MA, Mehdi A. Neck circumference as a useful marker of obesity: a comparison with body mass index and waist circumference. J Pak Med Assoc 2012; 62(1):36-40.
- Yang GR, et al. Neck circumference positively related with central obesity, overweight, and metabolic syndrome in Chinese subjects with type 2 diabetes: Beijing Community Diabetes Study 4. Diabetes Care. 2010; 33(11):2465-7.
- Misra A, Vikram NK. Insulin resistance syndrome (metabolic syndrome) and Asian Indians. Curr Sci 2002; 83:1483–96.
- Brusoni B, et al. Markers of inflammation, thrombosis and endothelial activation correlate with carotid IMT regression in stable coronary disease after atorvastatin treatment. Nutr Metab Cardiovasc Dis 2009; 19:481-90.
- Ervin RB. Prevalence of Metabolic Syndrome among Adults 20 Years of Age and Over, by Sex, Age, Race and Ethnicity, and Body Mass Index: United States, 2003–2006. National Health Statistics Reports No. 13. Hyattsville, MD: National Center for Health Statistics; 2009.
- Feng RN, Zhao C, Wang C, Niu YC, Li K, Guo FC, BMI is strongly associated with hypertension, and waist circumference is strongly associated with type 2 diabetes and dyslipidemia, in northern Chinese adults. J Epidemiol. 2012; 22(4):317-23.
- Onat A, Hergenç G, Yüksel H, Can G, Ayhan E, Kaya Z, et al. Neck circumference as a measure of central obesity:associations with metabolic syndrome and obstructive sleep apnea syndrome beyond waist circumference. Clin Nutr. 2009; 28(1):46-51.
- Deepa M, Farooq S, Datta M, Deepa R, Mohan V. Prevalence of metabolic syndrome using WHO, ATPIII and IDF definitions in Asian Indians: the Chennai Urban Rural Epidemiology Study (CURES-34) Diabetes Metab Res Rev. 2007;23:127-34.
- Gupte MD et al. The metabolic syndrome and associated risk factors in an urban industrial male population in South India. J Assoc Physicians India 2010; 58:363-6, 371.
- Fabregue G, et al. Relationship between neck circumference and hypertension in the National Hypertension Registry (the RENATA study). Revista Argentina De Cardiología 2012; 80(4):1-6.
- Lacobellis G, et al.Threshold values of high-risk echocardiographic epicardial fat thickness. Obesity (Silver Spring). 2008; 16(4):887-92.
- Sharma AM, et al. Relation of epicardial fat and alanineaminotransferase in subjects with increased visceral fat. Obesity 2008; 16: 179–83.
- Rutten A, et al. Peri-coronary epicardial adipose tissue is related to cardiovascular risk factors and coronary artery calcification in postmenopausal women. Eur Heart J 2008; 29:777–83.
Citation: Dr. Bobby Varghese, Dr. Rekha S Patil 2015. To study the relationship of neck circumference as a parameter in predicting metabolic syndrome- a one year cross sectional study, 2015;1 (1),22-31