| Sindhu B *1, Michael Selvaraj A2, Pavithra Lochani V3 |
| Authors: 1Assistant Professor, Spurthy College of Physiotherapy, Rajiv Gandhi University of Medical Sciences, Bangalore 2Associate Professor, Spurthy College of Physiotherapy, Rajiv Gandhi University of Medical Sciences, Bangalore. Corresponding Author: 3*Assistant Professor, Faculty of Physiotherapy, DR. M.G.R Educational and Research Institute, Chennai. Email ID: pavithralochani.physio@drmgrdu.ac.in |
ABSTRACT
| Objective: The objective of the study was to find out the effect of Functional Strengthening Exercise and conventional physiotherapy in motor performance of lower extremity in patients with middle cerebral artery stroke. The stroke patients have deficits in motor control and sensory system. Interventions like Task oriented exercises, strengthening programme, Neuro Developmental therapy (NDT) and Brunnstrom Movement therapy are required to achieve early recovery. Methodology: Thirty subjects were selected and divided into two groups based on selection criteria with age group between 45-55, both male and female, people affected by ischaemic stroke was included and those with cognitive deficits, visual and hearing disturbances, was excluded from the study. Pre-test was done by using Fugl-Meyer Motor Assessment (FMMA) – lower extremity as an outcome measure, proceeding with the treatment protocol; Group A: were the control group who received conventional physiotherapy. Group B: were the experimental group who received both task specific strengthening exercise programme along with conventional physiotherapy, treatment was given for 1 hour per day for 3 weeks. After the cessation of the treatment protocol, post-test was done using the same outcome measure. Result: Result of the study shows thattask specific strengthening exercise along with conventional therapy was effective in the Motor recovery of Lower extremity in patients with middle cerebral artery stroke. Conclusion: Functional training which concentrates on strengthening the muscles is an effective technique which can be easily applied in stroke clients. |
Keywords: Stroke, Task-Specific Strengthening Programme, Fugl-Meyer Motor Assessment (FMMA).
| Received on 16th February 2024; Revised on 23rd February 2024; Accepted on 27th February 2024. DOI:10.36678/IJMAES.2024.V10I01.001 |
INTRODUCTION
Stroke is one of the major health problems worldwide and an important cause of long-term disabilities, becoming a challenge for health. Many individuals may experience the recurrence of stroke, which is associated with more disabling conditions. A sedentary lifestyle and the presence of disabilities in individuals with stroke contribute to reduced physical activity levels and increased risks of cardiovascular diseases, declines in aerobic capacity, increased fatigue, and the development of new disabilities. Therefore, clinical rehabilitation guidelines for individuals recommend the maintenance of adequate physical activity levels, which are related to general well-being 1.
It represents the fourth cause of death worldwide and survivors present a combination of muscle weakness or imbalance, decreased postural control, muscle spasticity, poor voluntary control and body misalignments. The consequences of a stroke depend on its severity, brain location and type. The cerebral accidents can be classified into ischemic and hemorrhagic stroke; ischemic stroke comprises 87% of the cases and are caused by thrombotic occlusion of arteries and veins. Middle cerebral artery (MCA) is the largest cerebral artery commonly affected by cerebrovascular accidents. Patient recovery is highly dependent on age, gender and stroke severity (2).
Cerebrovascular disease is an important cause of illness in the elderly, and it causes serious developmental delays as well as disabilities. Up to 64% of patients who have experienced stroke have some degree of cognitive impairment. Stroke-related cognitive deficits affect the functional recovery and the benefits of rehabilitation. Likewise, the presence of cognitive impairment increases the risk of recurrent stroke, mortality, and diminishes the activities of daily living. The cognitive tasks and motor activities are important for the functional improvement in patients with neurological deficits. Therefore, it is necessary to consider both cognitive and motor training in rehabilitation therapy 3.
Impaired walking ability is a hallmark residual deficit following stroke. Although approximately 705 to 80% of adults who have survived a stroke will recover the ability to walk short distances on flat surfaces, 50% achieve limited community ambulation and 20% have unlimited ambulation in the community 4. In the early period of stroke, lower extremity (LE) paresis from impaired muscle activation limits the ability to advance the limb for swing and to support body weight during stance. Incomplete recovery and development of secondary impairments contributes to continued gait dysfunction 5.
Task-specific lower extremity training (TSLET) is a complex lower extremity exercise during which subjects learn about lower extremity movement while solving a problem using visual feedback. The TSLET is a relatively safe and easy method, which can be applied for stroke patients with low functional level (3). Task related training (TRT) is a rehabilitation strategy that involves goal-directed, functional movements in a natural environment to help patients derive optimal control strategies for alleviating movement disorders. It includes a wide range of interventions such as treadmill training, walking training on the ground, bicycling programmes, sit-to-stand exercises, and reaching tasks for improving balance 6. After stroke, task-related training improves the balance, mobility and performance of locomotor tasks more than other training interventions 7.
The Fugl-Meyer scale was developed as the first quantitative evaluative instrument for measuring sensorimotor stroke recovery. It is a well-designed, feasible and efficient clinical examination method that has been widely used among stroke population. It is highly recommended research tool for evaluating changes in motor impairment following stroke, with an excellent intrarater and interrater reliability with constructive validity 8.
The FM Scale is a 226-point multi-item Likert-type scale developed as an evaluative measure of recovery from hemiplegic stroke. It is divided into 5 domains: motor function, sensory function, balance, joint range of motion, and joint pain. Each domain contains multiple items, each scored on a 3-point ordinal scale (0 = cannot perform, 1 = performs partially, 2 = performs fully). The motor domain includes items measuring movement, coordination, and reflex action about the shoulder, elbow, forearm, wrist, hand, hip, knee, and ankle. The motor score ranges from 0 (hemiplegia) to a maximum of 100 points (normal motor performance), divided into 66 points for the upper extremity and 34 points for the lower extremity 9.
METHODOLOGY
Thirty subjects were selected and divided into two groups based on selection criteria with age group between 45-55, both male and female, people affected by ischaemic stroke-middle cerebral artery involvement and people who scored 6-12 in Fugl-Meyer Motor Assessment was included and those with cognitive deficits, aphasic conditions, visual and hearing disturbances, systemic disorder conditions was excluded from the study. The study was carried out at the Department of Neurology, out-patient unit of physiotherapy department, Sri Ramakrishna Hospital. Pre-test was done by using Fugl-Meyer Motor Assessment (FMMA) – lower extremity as an outcome measure, proceeding with the treatment protocol; Group A: were the control group who received conventional physiotherapy. Group B: were the experimental group who received both task specific strengthening exercise programme (standing and sitting down, isolated hip extension, coming up on toes, lateral walking in ramp with weight cuffs, forward step up, leaning sideways) along with conventional physiotherapy, treatment was given for 1 hour per day for 3 weeks. After the cessation of the treatment protocol, post-test was done using the same outcome measure. The statistics were done based on the data collected. The collected data were tabulated and analyzed using both descriptive and inferential statistics.
Intervention
Control Group: Conventional Physiotherapy
- Lying to sitting over side of the bed:
Patient rolled and assisted on to the sound side.
- Supine:
- Bridging-Affected leg is held steady at the knee and foot, patient lifts the buttocks off the bed.
- Bridging on the affected leg, patient lifts sound foot off the bed.
- Supine: Knee extension with Dorsiflexion.
Knee moved from full flexion into extension, foot held in dorsiflexion.
- Supine: Abduction and adduction control.
Patient lies with both legs flexed with his feet flat on the support, moves the sound leg into abduction and adduction while the affected leg is controlled.
- Icing to Facilitate Dorsiflexors.
- Activities in sitting: Weight transference in sitting to the affected side and to the sound side, feet unsupported.
- Sitting to Standing:
Pelvis supported, legs, wedge the patient’s feet and knee. Patient instructed to lean forward at the hip.
- Squatting activity with wall bar support.
- Standing:
- Weight transference to the affected and to the sound side.
- Weight bearing on the affected leg, patient supported on the affected side and instructed to place the sound leg over a step.
- Affected leg placed on a step patient shifts weight well Forward, steps upon to it.
- Patient practices stepping down with the sound leg.
Experimental Group: Task Specific Strengthening Exercise:
Standing and sitting down:
Sitting feet flat on the floor patient practices inclining trunk forward by flexing at the hip with neck and trunk extension with enough momentum to move the knees forward with shoulders and knee forward patient practices standing up (Heel moved 10cm towards chair). Standing up done with shoulders flexed to 90 degrees with elbow in flexion.

Figure 1
- Isolated Hip Extension:
Prone lying on the bed, the affected foot is placed over stool and isolated hip extension performed.
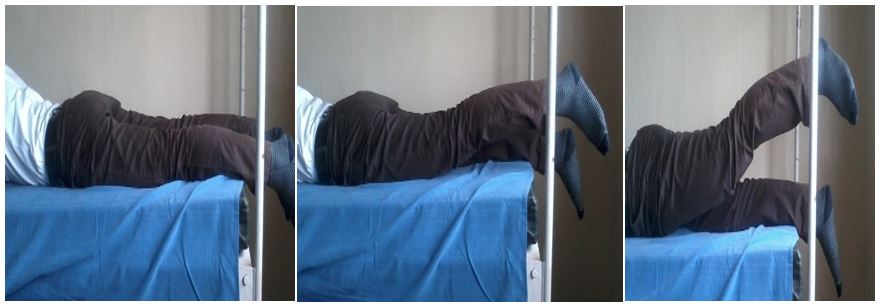
Figure 2
- Coming Up on Toes:
Standing at the edge of the foot stool patient advised to lower both heels and to lift the heels and to lift the heels up.

Figure 3
- Lateral Walking In Ramp:
Weight cuffs applied to affected leg just above the ankle and patient advised lateral walking in ramp.
 Figure 4
Figure 4
- Forward Step Up:
The affected foot placed over the stool and patient advised to step up over the stool.

Figure 5
- LATERAL SITTING:
Sitting on the mat patient advised to get up and sit as if giving way to next person. Lateral sitting to right and to the left.
 Figure 6
Figure 6
Table-1 Comparison of Fugl-Meyer Motor Assessment (FMMA) – Lower Extremity Between Pre-Test and Post-Test Within Group A
| GROUP – A | PRE-TEST | POST-TEST | t – TEST | |||
| MEAN | S.D | MEAN | S.D | SIGNIFICANCE | ||
| FMMA | 8.931 | 1.667 | 27.32 | 1.927 | 3.070 | 0.000*** |
The above table reveals the Mean, Standard Deviation (S.D), t-test, and p-value of the FMMA between pre-test and post-test. Within GROUP A (***- P ≤ 0.001)
There is statistically highly significant difference between the pre-test and post-test values within GROUP A (***- P ≤ 0.001)
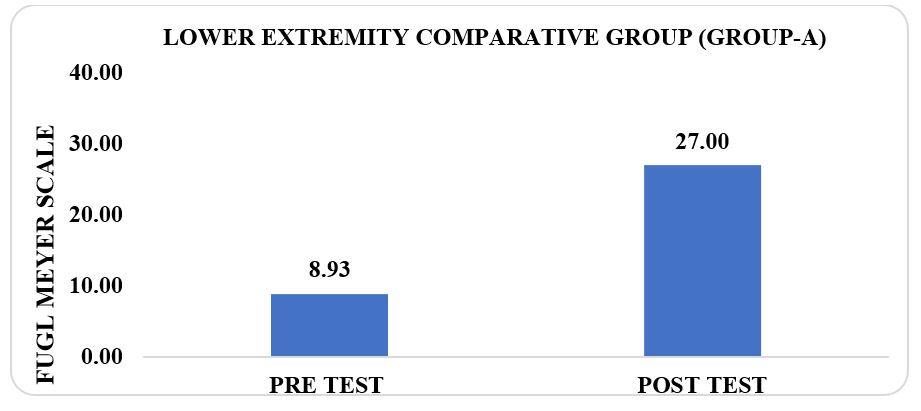
Graph-1 Comparison of Fugl-Meyer Motor Assessment (FMMA) – Lower Extremity Between Pre-Test And Post-Test Within Group A
Table-2 Comparison of Fugl-Meyer Motor Assessment (FMMA) – Lower Extremity Between Pre-Test and Post-Test Within Group B
| GROUP – B | PRE-TEST | POST-TEST | t – TEST | |||
| MEAN | S.D | MEAN | S.D | SIGNIFICANCE | ||
| FMMA | 8.933 | 1.669 | 28.93 | 1.032 | 3.070 | 0.000*** |
The above table reveals the Mean, Standard Deviation (S.D), t-test, and p-value of the FMMA between pre-test and post-test. Within GROUP B (***- P ≤ 0.001)
There is statistically highly significant difference between the pre-test and post-test values within GROUP B (***- P ≤ 0.001)
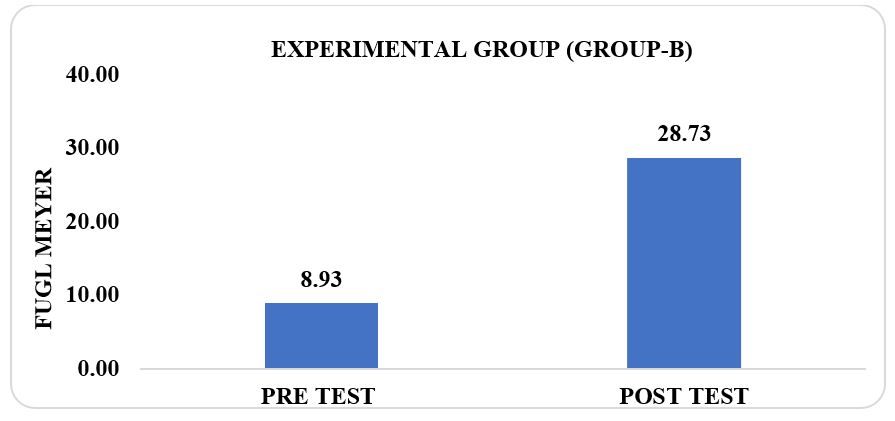
Graph-2 Comparison of Fugl-Meyer Motor Assessment (FMMA) – Lower Extremity Between Pre-Test and Post-Test Within the Group
Table- 3 Comparison of Fugl-Meyer Motor Assessment (FMMA) – Lower Extremity Between Group A & Group B In Pre-Test and Post-Test
| #FMMA | #GROUP – A | #GROUP – B | t – TEST | ||||
| MEAN | S.D | MEAN | S.D | df | SIGNIFICANCE | ||
| PRE-TEST | 8.93 | 1.667 | 8.93 | 1.669 | 0.007 | 28 | 0.989 |
| POST TEST | 27.32 | 1.927 | 28.93 | 1.032 | 3.070 | 28 | 0.004*** |
GROUP A – Conventional Therapy & Group B – Task-Specific Strengthening Exercise
The above table reveals the Mean, Standard Deviation (S.D), t-test, degree of freedom and p-value of the FMMA between (Group A) & (Group B) in pre-test and post-test.
This table shows that there is no significant difference in pre-test values of the FMMA between Group A & Group B (*P > 0.05).
It shows that statistically highly significant difference in post-test values of the FMMA between Group A& Group B (***- P ≤ 0.001)

Graph-3 Comparison of Fugl-Meyer Motor Assessment (FMMA) – Lower Extremity Between Group A & Group B In Pre-Test and Post-Test
RESULT
The collected data were tabulated and analyzed using both descriptive and inferential statistics. Paired t-test was adopted to find the statistical difference within the groups & Independent t-test (Student t-Test) was adopted to find the statistical difference between the groups.
From the data analysis, on comparing Group A and Group B who underwent Conventional Training and Task-Specific Strengthening Training obtained the mean difference of (18.07) & (19.80) in Fugl-Meyer Motor Assessment (FMMA) – Lower Extremity respectively. Group A and Group B reveals that ‘t’ value of FMMA (0.008) & (3.070), p value of FMMA (0.0001***) & (0.0001***) respectively. Both groups show p value (p ≤ 0.001), however Group B shows more significant than group A. Hence the study accepts the alternate hypothesis and rejects null hypothesis.
DISCUSSION
Stroke is one of the major health problems with long-term disabilities (1). It represents the fourth cause of death worldwide and survivors present with muscle weakness or imbalance, decreased postural control, muscle spasticity (2). Impaired walking ability is a hallmark residual deficit following stroke. Incomplete recovery and development of secondary impairments contributes to continued gait dysfunction. Muscle strength training may lead to improvement in both lower-limb strength and gait speed in patients with stroke (4).
Evidence from various studies reported that task specific strengthening exercises has been shown to improve lower limb motor performance in subjects with stroke.
Katherine J. Sullivan et al (2011)., concluded that the task specific and body weight supported treadmill walking is highly beneficial to stroke clients. Task-specific training found to be effective in improving the mobility in individuals with stroke, stated by Sylvie Nadeau et al (2017).
Task Specific Lower Extremity Training (TSLET) had a significant effect on cognitive and gait function compared with conventional physical therapy in patients with subacute stroke. It could be an effective strategy for improvement in cognitive, gait and balance functions in stroke patients., concluded by Sae Hoon C et al., (2019)
Suraj Bhimrao Kinase et al. (2014) did a study on “Effect of task related training versus conventional training on walking performances in post Stroke patients”, the study concluded that task related training was significantly effective in improving walking performances and conventional training was effective in reversing the speed.
The above discussions provide evidence that both conventional therapy and task specific strengthening exercise individually improves lower limb motor performance in subjects with stroke. In the present study, we had implemented both to compare the effectiveness among these exercises. The data analysis and statistic interference have brought to check the effectiveness of task specific strengthening and conventional therapy in lower limb motor performance in subjects with stroke.
In the study, GROUP-A (control group) which underwent for conventional therapy and GROUP-B (experimental group) which underwent for task-specific strengthening programme, both had a significant improvement in improving lower limb motor performance in stroke patients.
The mean value of FMMA between Group A pre-test mean value (8.931) and post-test mean value (27.32) showed a significant difference. The mean value of FMMA between Group B pre-test mean value (8.933) and post-test mean value (28.93) showed a significant difference. It was evident from the mean difference that both groups showed improvement in the FMMA (Fugl-Meyer Motor Assessment).
Result of the present study showed patients of Group B treated with Task-Specific Strengthening exercise as shown a significant improvement (P<0.001). the unpaired ‘t’ test of group A and Group B reveals that ‘t’ value of FMMA (0.008) & (3.070) respectively. This may help the stroke patient to improve their quality of life by improving their lower limb motor performance.
Our data supported alternate hypothesis that task specific strength training programme was more effective than conventional therapy in the motor recovery of lower extremity in patients with middle cerebral artery stroke. Hence, null hypothesis is rejected.
Conflict of Interest: The authors declared that they have no conflicts of interest and no funding has been obtained from any source.
CONCLUSION
Conclusion of the study shows that task specific strengthening exercise and conventional therapy were effective in improving the lower limb motor performance in stroke patients. Functional training which concentrates on strengthening the muscles is an effective technique which can be easily applied in stroke clients. This technique trains the lower limb muscles both Eccentrically and Concentrically. Bio mechanical studies prove that eccentric strengthening exercise is highly beneficial than other forms of strengthening programmes.
Task specific strengthening exercise applied in stroke patients prove that they are highly beneficial than the conventional technique. Therefore, the present study concluded that task specific strengthening programme along with coventional therapy was better in the motor recovery of lower extremity in patients with middle cerebral artery stroke when compared with the group which underwent only conventional therapy.
Authors Contribution: Dr. Michael selvaraj A and Dr. Sindhu B conceived and designed the analysis and collected the data. Dr. Pavithra Lochani V, participated in the design of the study, Performed the statistical analysis and contributed to draft the manuscript.
REFERENCES
- Júlia Caetano Martins, Larissa TA, Sylvie Nadeau, Aline AS, LF Teixeira-Salmela, Christina Danielli CD. Efficacy of Task-Specific Training on Physical Activity Levels of People with Stroke: Protocol for a Randomized Controlled Trial. Phys Ther. 2017; 97:640–648.
- Anselmo de Athayde CS, Cardoso Nascimento, Ramon Costa de Lima. Positive balance recovery in Ischaemic Post-Stroke patients with Delayed Access to Physical Therapy. BioMed Research International. 2020; 9153174.
- Sae Hoon C, Ji Hyun Kim, Sang Yeol Yong, Young HL, Jung Mee Park, Sung Hoon Kim, Chan Lee. Effect of Task-Specific Lower Extremity Training on Cognitive and Gait Function in Stroke Patients: A Prospective Randomized Controlled Trial. Ann Rehabil Med. 2019; 43(1):1-10.
- Katherine J Sullivan,David A Brown, Tara Klassen, Sara Mulroy, Tingting Ge, Stanley P Azen, Carolee J Winstein. Effects of Task-Specific Locomotor and Strength Training in Adults Who Were Ambulatory After Stroke: Results of the STEPS Randomized Clinical Trial. Physical Therapy, 2007, Volume 87(12):1580–1602.
- De Quervain IA, Simon SR, Leurgans. Gait pattern in the early recovery period after stroke. J Bone Joint Surg Am. 1996; 78:1506 –1514.
- Shweta Vijay Ghag, Suvarna Shyam Ganvir. Task-Oriented Training in Rehabilitation of Gait After Stroke: Systematic Review. Journal of Medical Biomedical and Applied Sciences. 2018 Vol 6 No 3.
- Lee HS, Kim MC. The effects of balance task-related circuit training on chronic stroke patients; J Kor Soc Phys Therapy. 2009; 21:23-30.
- David J Gladstone, Cynthia J Danells, Sandra E Black. The Fugl-Meyer Assessment of Motor Recovery after Stroke: A Critical Review of its Measurement Properties. Neurorehabilitation and neural Repair. 2002;16(3):232-40.
- Katherine J Sullivan, Julie K Tilson, Steven Y Cen, Anita Correa, Joann Gallichio. Fugl-Meyer Assessment of sensorimotor function after stroke. 2010; 42:427-432.
- SB Kinase, G Varadharajalu. Effect of Task Specific Training versus Conventional Training on walking performance in post-stroke patients. International journal of Science and Research; 2014; vol 3 issue 11, 2786-2790.
- Wagenaar RC, an Wieringen PC, Netelenbos JB, Meijer OG, Kuik DJ. The transfer of scanning training effects in visual inattention after stroke: five single-case studies. Disabil Rehabil. 1992; 14: 51–60.
- Kwakkel G, Wagenaar RC, Twisk JW, Lankhorst GJ, Koetsier JC. Intensity of leg and arm training after primary middle-cerebral-artery stroke: a randomised trial. Lancet. 1999; 17: 354:191–196.
- Pollock A, Baer G, Pomeroy V, Langhorne P. Physiotherapy treatment approaches for the recovery of postural control and lower limb function following stroke. Cochrane Database Syst Rev. 2007; 1: CD001920.
- Paci M. Physiotherapy based on the Bobath Concept for adults with post-stroke hemiplegia: a review of effectiveness studies. J Rehabil Med. 2003; 35:2–7.
- Van Peppen R, Kwakkel G, Wood-Dauphinee S, Hendriks H, Van der Wees P, Dekker J. The impact of physical therapy on functional outcomes after stroke: what’s the evidence? Clin Rehabil.2004; 18: 833–862.
| Citation: Sindhu B, Michael Selvaraj A, Pavithra Lochani V (2024). Efficacy of Task Specific Strength Training to Improve Lower Limb Motor Performance in Subjects with Stroke, ijmaes; 10(1); 1723-1732 |

Leave a Reply