James W H Manik1, Beriman Rahmansyah2
Corresponding Author:
1Lecturer, Faculty of Vocational Studies, Physiotherapy Program, Universitas Kristen Indonesia, Jakarta, Indonesia, Email: jamesmanik@uki.ac.id
Co-Author:
2Lecturer, Faculty of Vocational Studies, Physiotherapy Program, Universitas Kristen Indonesia, Jakarta, Indonesia
ABSTRACT
Background: Neuromobilization is a technique which is an application of manual therapy focused on nerve fibers with a sliding and stretching mechanism. Currently, it is often used as a form of diagnosis and treatment of musculoskeletal conditions with involvement of the nervous system. Increased nerve flexibility will reduce nerve sensitivity to painful stimuli. The use of transcutaneous electrical stimulation (TENS) electric currents in conditions of nerve disorders can help eliminate/reduce pain symptoms if the area given the TENS current has normal nerve sensitivity. This study aims to determine the effect of median neuromobilization on the perception of pain from electrical stimulation in the body parts innervated by the median sensory nerve.
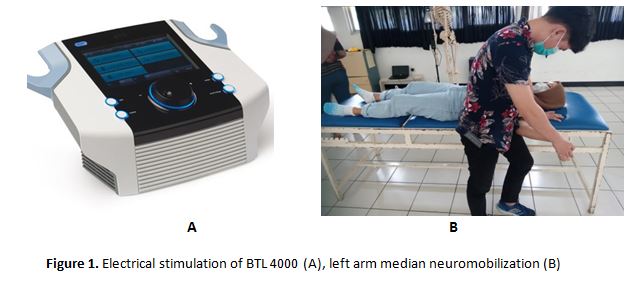
Method: This study is an experimental research with Single Group Pretest Posttest Design. A research group with a subject of 50 people who will be measured electrical pain perception before and after being given neuromobilization. Pain perception examination was carried out by providing electrical stimulation to the left forearm using an electrical stimulation device brand BTL 4000 with a dynamic current type, constant current intensity 5Hz in 3 minutes. The instrument used to measure pain perception is the visual analog scale (VAS).
Results: Hypothesis testing with the Wilcoxon signed ranks test showed a significant decrease in pain perception after neuromobilization of the median nerve to the sample with a Z value of -2,956 and a p value (Asymp Sign. 2-tailled) of 0.003 (˂ 0.05).
Conclusion: Mobilization of the median nerve can significantly reduce the perception of electrical pain in the skin area innervated by the C6, C8 and Th1 spinal cord segments and the median nerve (palmar surface of the left forearm 1/3 distal and thenar area)
Keywords: Median nerve mobilization, Pain perception, Physiotherapy, Neuromuscular
Received on 17th August 2021, Revised on 27th August 2021, Accepted on 31ST August 2021, DOI:10.36678/IJMAES.2021.V07I03.009
INTRODUCTION
Pain is an unpleasant sensory and emotional experience resulting from actual or potential tissue damage or described in terms of the damage1. The mechanism of pain is based on multiple processes, namely nociception, peripheral sensitization, phenotypic changes, central sensitization, ectopic excitability, structural reorganization, and decreased inhibition. The perception of pain felt by individuals without being caused by tissue damage can be controlled, and this does not apply to pain that arises due to tissue damage2.Most of the tissue pathological conditions associated with movement and function disorders cause pain complaints, both acute pain and chronic pain3.
Carpal Tunnel Syndrome (CTS)is a condition of the median nerve disorder with symptoms of pain or tingling due to compression of the median nerve around the wrist in the carpal tunnel area4. Pressure on the median nerve can result from repetitive wrist movements or holding the wrist still in an improper position. One way to overcome pain due to tissue damage is to use a TENS (transcutaneous electrical nerve stimulation) device by modifying the appropriate current in the form of electrical stimulation to stimulate sensory nerve fibers that receive pain stimuli5.
Apart from being an intervention modality to reduce pain, TENS can also be used to measure the level of nerve sensitivity, especially sensory nerves. So that the use of TENS as an intervention modality should begin with measuring the level of nerve sensitivity related to the pain to be overcome. The low nerve excitability brother illustrates that the condition of the nerve sensitivity is high. In other words, the perception of pain is high. This becomes an obstacle in TENS intervention to reduce pain in a condition. For this reason, it is necessary to carry out an intervention that aims to reduce nerve sensitivity so that the perception of stimuli becomes normal, one of which is the electrical stimulation generated from TENS6.
High nerve sensitivity can be caused by the structure of the neural network itself (intra-neural) and other tissues around the nerves (extra-neural) which, when experiencing a decrease in flexibility, can increase the sensitivity of the nerve.Neuromobilization is a technique which is a application of manual therapy focused on nerve fibers with a sliding and stretching mechanism7.
Neuromobilization techniques are passive or active movements that are focused on restoring the ability of the nervous system to tolerate normal compressive, frictional, and pulling forces associated with daily activities and sports 8. Neuromobilization is an intervention aimed at restoring homeostasis in and around the nervous system, by mobilizing the nervous system itself or the structures surrounding the nervous system9.
This study aims to determine the effect of median neuromobilization on the perception of pain from electrical stimulation in the body parts innervated by the median sensory nerve. A similar study was conducted by Beneciuk, et al2with the title Effects of Upper Extremity Neural Mobilization on Thermal Pain Sensitivity: A Sham-Controlled Study in Asymptomatic Participants to determine the effect of median neuromobilization on temperature perception in the area innervated by the median nerve by providing hot water (temperature 70 degrees celsius) on the skin innervated by the median nerve as a heat stimulus using a visual analog scale (VAS) instrument and concluded that there was a decrease in the perception of heat sensation in the skin area innervated by the median nerve after median neuromobilization. However, the decrease in heat sensation is temporary. However, in this study, mobilization of the median nerve was carried out to determine its effect on the perception of electrical stimulation of pain by providing an electric current of 5Hz intensity TENS type continuous current type in the area of the skin innervated by the median nerve and measuring the perception of electrical stimulation pain using a visual analog scale (VAS) instrument. Examination of the median nerve tension is the initial stage that will be carried out before providing neuromobilization to determine the level of nerve sensitivity to be given.
METHODS
This study is an experimental research with Single Group Pretest Posttest Design. A research group with a subject of 50 people who will be measured electrical pain perception before and after being given neuromobilization.Pain perception examination was carried out by providing electrical stimulation to the left forearm using an electrical stimulation device brand BTL 4000 with a dynamic current type, constant current intensity 5Hz in 3 minutes. The instrument used to measure pain perception is the visual analog scale (VAS).
The range of pain is represented as a line 10 cm long, with or without markings per centimeter. The marks at either end of this line can be numbers or descriptive statements. One end represents no pain, while the other end represents the worst possible pain.Median neuromobilization was carried out to the sample in the supine position on the bed with the arm in the scapular depression position, the shoulder abducted at 90, maximal shoulder external rotation, maximum elbow extension, wrist and finger extension. Then the elbow joint is passively extended in accordance with the pain tolerance felt by the sample and the wrist is repeated 10 times. Neuromobilization was performed 3 times a week for 4 weeks.This study was obtained ethical clearance from Universitas Kristen Indonesia with reference number 08/Etik Penelitian/FKUKI/2020.
RESULT
Median Neuromobilization Research for Faculty Vocational studies students has been carried out for 1 month (19 November – 18 December 2020). The number of samples is 47 people.
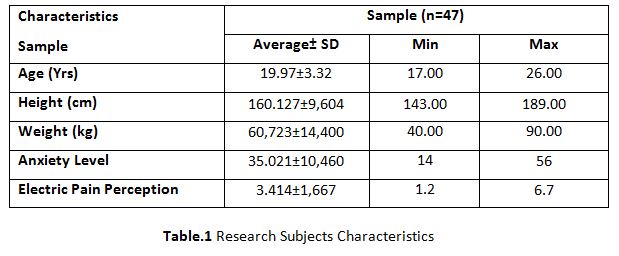
Table 1 shows the average height of the sample 19.97±3.32, weight 60, 723± 14,400, anxiety level 35,021±10,460 and perception of electrical pain stimulation 3,414±1,667. The average level of anxiety (35,021) is included in the category of severe anxiety and the average perception of electrical pain (3,414) is included in the category of mild pain.
Normality test: To determine the type of comparative statistical test to be used which aims to compare the results of the pre-test and post-test in the paired group, the data normality test was first performed using the Saphiro Wilk Test.
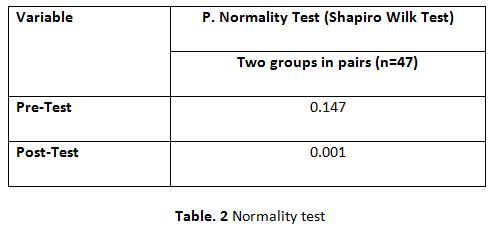
Table 2 shows that the results of the normality test using the Shapiro Wilk Test on the pre-test and post-test variables of the two paired groups were not normally distributed where the pre-test p value = 0.147 (p 0.05) and post-test = 0.001 (p 0.05). 0.05) ,test the mean difference of two groups in pairs.
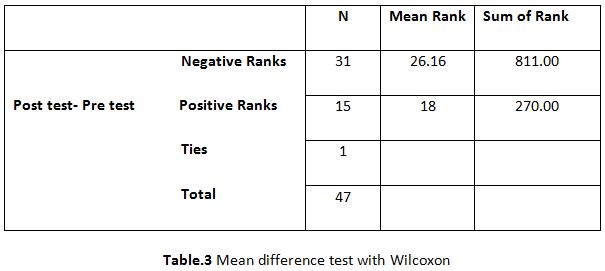
Table.3 shows the results of the two-group mean difference test in
pairs before and after the intervention. The negative ranks value of 31
indicates that there are 31 samples experiencing a decrease in pain perception after
neuromobilization with a mean
rank of 26.16. While the positive ranks value of 15 shows that as many as 15
samples experienced an increase in pain perception with an average (mean ranks)
of 18. Ties 1 indicate that there is 1 sample that did not experience a change
in the value of pain perception after neuromobilization.
Pain Perception Hypothesis Test
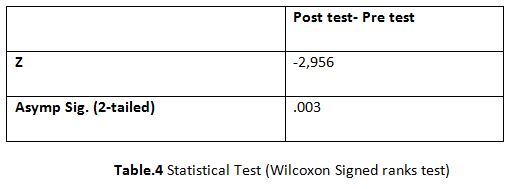
From the results of hypothesis testing with the Wilcoxon signed ranks test in table 4, it shows a significant decrease in pain perception after mobilizing the median nerve to the sample with a Z value of -2,956 and a p value (Asymp Sign. 2-tailled) of 0.003 (˂ 0.05).
DISCUSSION
In this study, it was concluded that the median nerve neuromobilization in 47 study samples could significantly reduce the perception of electrical pain in the skin area innervated by the C6, C8, and Th1 spinal cord segments and the median nerve (palmar surface of the left forearm 1/3 distal to the spinal cord and thenar area). These results indicate that the mobilization of nerves by using the technique of stretching the median nerve and shearing of nerves with adjacent structures of the nervous system will affect the sensitivity of the nervous tissue. Median neuromobilization intervention was given 3 times a week for a month. Electrical stimulation with a diadynamic current type, constant current intensity of 5Hz for 3 minutes aims to cause electrical pain in the first minute then causes pain until the third minute.
There were 4 samples experienced erythema on the skin surface of the hypothenar area of the hand but a few hours later the erythema disappeared. While the other samples did not cause changes to the skin surface. This result is in line with a similar study entitled Effects of Upper Extremity Neural Mobilization on Thermal Pain Sensitivity: A Sham-Controlled Study in Asymptomatic Participants.The results obtained from the study that compared the effect of the actual neuromobilization technique and the pseudo-neuromobilization was a significant decrease in the perception of hot temperature stimulation in the skin area innervated by the median nerve with temperature stimulation of 49° temporally summation on the actual neuromobilization technique with p value 0.0322.
The importance of nerve tissue sensitivity and the slipping effect in adjacent structures of the nervous system, suggests that the neuromobilization test distinguishes normal from abnormal neural tissue, by means of its sensitivity mechanics. neuromobilization can also restore a dynamic balance between the relative motion of the neural network and the surrounding mechanical interface, thereby enabling the intrinsic stress on the neural network to be optimal. Decreased blood supply to nerves due to decreased vasodilation in blood vessels that supply nerves can cause hypersensitivity in these nerve pathways7.
Mobilization of the median nerve can also affect the perception of the threshold of vibration stimulation as previous studies in knowing the Effect of neuromobilization on Altered Vibration Perception Threshold (VPT)10.A total of 6 times the mobilization of the right median nerve which was previously measured by the perception of the vibrational threshold using a bioesthesiometer was given to the thumb of the right hand. The measurement of the vibration threshold with a bioesthesiometer is able to provide vibrations at a constant frequency of 100Hz.
Vibration stimulation is given by increasing the intensity until the thumb feels the vibration, then decreasing the intensity until the thumb does not feel the vibration. Furthermore, the intensity of the vibration is increased again to the first point where the vibration is felt. The experiment was carried out three times, and the mean of the values from the three trials was recorded as the threshold value for vibration perception. The results of this study indicate a significant decrease in the threshold of vibration stimulation at p value 0.001 (p˂0.05).
Intraneural movement restriction (Endoneurium, epineurium & perineurium) is a conduit of the meninges (dura mater, arachnoidea, pia mater) and extraneural (tissue that is near the nerve tissue in the form of fascia sheaths, blood vessels, muscles, ligaments, bones) will be detected by a tension testin which high nerve sensitivity is characterized by the onset of stretching pain.
neuromobilization has a direct effect on nerve conduction as measured by electro-physiological examination, thus providing evidence for including neuromobilization as an intervention in altered neuromobilization in peripheral nerves8.
One of the goals of neuromobilization is to restore homeostasis around the targeted nerve11. There are also other studies that compare the effect of neuromobilization with neural gliding and neural tension techniques on the threshold for perception of tenderness and temperature12.
The results found from this study were that there was a significant difference in the reduction in pain and temperature perception thresholds between the neural gliding and neural tension techniques, in which the neural gliding technique was superior.
Neuromobilization is commonly applied to patients with lumbar radiculopathy, carpal tunnel syndrome and other peripheral nerve problems13. Application of neuromobilization in Carpal Tunnel Syndrome (CTS) conditions in a study that compared the effects of treatment on median neuromobilization, carpal bone mobilization and untreated CTS conditions. Each group consisted of 7 patients who had CTS14.
The results obtained from this study are that neuromobilization can reduce pain in CTS in both treatment groups compared to the untreated group (p=0.01). However, in the exploration of the results of the two treatment groups there was no statistically significant difference.
The effect of neuromobilization on significant pain reduction in combination with the provision of a splint in CTS conditions was also proven in a study entitled Effect of neural mobilization and splinting on carpal tunnel syndrome4.
The first group in this study was only given splinting for 3 weeks, while the second group, apart from being given splinting, also underwent neuromobilization. There was a significant reduction in pain in the splinting and neuromobilization group with pain measurement instruments using the visual analog scale (VAS) and the Boston Questionnaire Symptom Severity Scale.
Peripheral nerves may be subjected to mechanical or chemical irritation at different anatomic points along their course. Prolonged nerve compression or fixation may result in decreased intraneural blood flow15. This then triggers the release of pro-inflammatory substances (peptides linked to the calcitonin gene and substance P) from the nerves. This byproduct is referred to as neurogenic inflammation and can interfere with normal nerve function even without marked nerve damage, it can also contribute to the initiation and spread of chronic pain16.
This study was experimental study, so, in the future need to conduct more comprehensive study to know the best effect of neuromobilization in pain perception.
CONCLUSION
Mobilization of the median nerve can significantly reduce the perception of electrical pain in the skin area innervated by the C6, C8, and Th1 spinal cord segments and the median nerve (palmar surface of the distal 1/3 left forearm and thenar area).
Ethical clearance: Ethical clearance obtained from Faculty of Medicine, Universitas Kristen Indonesia, Jakarta, Indonesia
Conflict of interest: The author has no conflict of interest to declare.
Funding of study: This study was funded by Universitas Kristen Indonesia.
REFERENCE
1. Bahrudin M. Patofisiologi Nyeri (Pain). Saintika Med. 2018;13(1):7. doi:10.22219/ sm.v13i1.5449.
2. Beneciuk JM, Bishop MD, George SZ. Effects of upper extremity neural mobilization on thermal pain sensit-ivity: A sham-controlled study in asymptomatic participants. J Orthop Sports Phys Ther. 2009; 39(6); 428-438.
3. Basson A, Olivier B, Ellis R, Coppieters M, Stewart A, Mudzi W. The effectiveness of neural mobiliz tion for neurmusculoskeletal conditions: A systematic review and meta-Analysis. J Orthop Sports Phys Ther.2017; 47(9),593-615.
4. Manchanda V. Effect of neural mobilization and splinting on carpal tunnel syndrome Article Information. J Heal Sci Dev J Heal Sci Dev. 2020; 3:1-10.
5. Al-zamil M, Ng K. TENS and Acupuncture in treatment of Carpal Tunnel Syndrome. Int J Pharmacogn Chinese Med. 2021; 5(1); 1-4. doi:10. 23880/ipcm-16000210
6. Siddiqui A, Dentist P, Practitioner P. Comparative Evaluation of Transcutaneous Electronic Nerve Stimulation and Topical Anesthesia in Reduction of Pain Perception during Administration of Local Anesthesia in Pediatric Dental Patients.2021; 25(6); 1793 -1798.
7. Shacklock M. Clinical Neurodynamics. Elsevier Ltd; 2005.
8. Kumar V, Goyal M, Rajendran N. Effect of neural mobilization on monosynaptic reflex-A pretest post test experimental design. Int J Physiother Res. 2013; 3(3); 58-62.http://www. ijmhr.org/ijpr_articles.
9. Henrique H. Neurodynamic Mobilization and Peripheral Nerve Regeneration: A Narrative Review. Int J Neuror ehabili tation. 2015; 02(02). doi:10.4172/ 2376-0281.1000163.
10. Manisha P, Ganesh B, Ravi S. Effect of Neural Mobilization on Altered Vibration Perception Threshold (VPT). Indian J Physiother Occup Ther. 2011;5(2):85-88.
11. Boyling JD, Jull GA, eds. Grieve’s Modern Manual Therapy. 3rd ed. Churchill Living Stone Elsevier; 2004.
12. Martins C, Pereira R, Fernandes I, et al. Neural gliding and neural tensioning differently impact flexibility, heat and pressure pain thresholds in asymptomatic subjects: A randomized, parallel and double-blind study. Phys Ther Sport. 2019; 36; 101-109.
13. Shacklock M. Clinical Neurodynamics Course Manual. Neurodynamic Solut Adelaide, Aust. Published online 2005.
14. Tal-Akabi A, Rushton A. An investi-gation to compare the effectiveness of carpal bone mobilisation and neuro-dynamic mobilisation as methods of treatment for carpal tunnel syndrome. Man Ther. 2000; 5(4); 214-222.
15. Bove GM, Delany, Sean P, Hobson L, et al. Manual therapy prevents onset of nociceptor activity, sensorimotor dysfunction, and neural fibrosis induced by a volitional repetitive task. Pain. 2019; 160(3); 139-148. doi: 10.1097/j. pain. 00 1443. Manual.
16. Matsuda M, Huh Y, Ji RR. Roles of inflamm ation, neurogenic inflammaion and neuro inflammation in pain. J Anesth. 2019; 33(1); 131-139. doi:10.1007/s00540-018-2579-4.
| Citation: James W H Manik, Beriman Rahmansyah(2021). The effect of nerve mobilization on the median nerve in pain perception of electrical stimulation, ijmaes; 7 (3); 1104-1112. |

Leave a Reply