Ochala Ejura Jennifer1, Rauf Ibrahim2,Samsiah Mat3, Syed Ali Gulab Jan4
Authors
1Graduate, School of Nursing, MAHSA University, Malaysia, Senior Nursing Officer, Federal Medical Centre Abuja, Nigeria, West Africa,
Email: ejujennifer@yahoo.com
2Department of Statistics, Faculty of Science, University of Abuja, Nigeria, West Africa.
Email id: rauf.ibrahim@uniabuja.edu.ng
4Professor, M.N.R. College of Nursing, Narsapur Road, Fasalwadi, Sangareddy, Telengana, India
Corresponding Author
3Associate Pofessor, School of Nursing, MAHSA University, Selangor, Malaysia
Email Id: samsiah7381@gmail.com
ABSTRACT
Introduction: Nigeria is the 4th highest contributor to global maternal mortality; many postpartum mothers do not initiate contraceptives early and are at increased risk of unplanned pregnancy and abortion. Understanding the barriers is thus vital. This cross-sectional quantitative study carried out at a tertiary hospital in Abuja to determine the contraceptive practice level, identify barriers to use among mothers with infants less than 12 months.
Methodology: Questionnaires were administered on 220 consenting mothers; data analyzed using SPSS software version 25. Descriptive analysis included frequencies and percentages, the inferential statistical techniques used are binary logistic regression to establish the relationship between variables — the p-value set at 5% level, thus p<0.05 is termed significant.
Results: 200 questionnaires were retrieved; the mean age of the respondents was 31; most had tertiary level education, were in monogamous union and Christians. Over-half is within 3months postpartum and desired to have below four children. The commonly used methods are the condom, IUD, pills and implant. 48% are currently on a method, and 1% less have good contraceptive practice. Identified barriers are personal information and health system barriers. Barriers associated with the health system found to impact on the use of contraceptives (p=0.028). Contraceptive use was dependent on respondent’s religion (p=0.050) and child’s age (p=0.038).
Conclusion: Contraceptive practice level of respondents is less than average and child’s age and religion determined it, the mothers are indifferent on personal information and family/cultural barriers, but concerned on health system barriers. Tackling health system barriers in the postpartum period through early education, counseling, opening and equipping more family planning clinics and health facilities can improve contraceptive use.
Keywords: Contraceptive practice, Barriers, Postpartum mothers
| Received on 25th September 2020, Revised on 16th October 2020, Accepted on 18th November 2020 |
DOI:10.36678/IJMAES.2020.V06I04.002
INTRODUCTION
Family planning involves a conscious decision by persons in the reproductive age group to control space or limit childbirth. Globally, the challenge associated with high birth rate is enormous. International reports show that 190 million women of reproductive age do not want to get pregnant yet do not employ any modern contraceptive method. Meeting the Sustainable development goal (SDG) 3.1 and 3.7 of reducing maternal mortality and increasing proportion of women with satisfied contraceptive need plus increased access to reproductive health service might be a mirage with non-use of contraceptives 1, 2 .
Increased access to contraceptives in the post-delivery period can increase the gains of reduced maternal mortality, unintended pregnancies, associated induced abortions and the proportion of high-risk pregnancies. It is also capable of reducing the already heightened pressure on Nigeria’s resource and produce direct benefit on social, health and financial investment 3,4,5.
The estimates (2000-2017) shows Nigeria is the 4th highest contributor to maternal mortality rate (MMR) in the world after Sierra Leone, Chad and Sudan at 917 per 100,000 live births and has witnessed a marginal 24% change in MMR between 2000 and 2017; this reflects the quality of maternal and child care provided 6, 7.
The Federal Ministry of Health Nigeria set 2014-2018 as the period to double the contraceptive prevalence to 36%. There appeared marginal increase in the west (Lagos) and north (Kaduna) howbeit only 15.6% of women within 15-49 years use any method of contraception, 23% of women in the north central zone have an inter-pregnancy interval of less than 23months, yet 23% do not want to have more children 8,9, 10.
Moreover, research done in Abuja revealed contraceptive use among women is below average (38-42%) whereas there are reports of unintended pregnancy (16%) with 80% having misconception and fears about the modern methods4,11,12. There appear a widespread fear of side-effects, misconception and social restriction regarding contraceptive use among women. They desire to make a rational decision about family size and timing of pregnancy, however, are constrained by lack of spousal consent, cultural, religious and educational inhibition 13, 14.
Thus, the need to investigate and delineate contraceptive practice level and barriers associated with input from the mothers in a health facility that offers this service in Abuja. This study aims to investigate the contraceptive practices, specific barriers to utilization of contraceptives among women within 12months after delivery.
METHODOLOGY
This study is a descriptive, cross-sectional study to evaluate the practices, barriers, to contraceptive use among mothers attending the immunization clinic of the University of Abuja Teaching Hospital (UATH), Gwagwalada. The accessible population is about 1,960 Nigerian mothers 18-49 years with an infant below 12months attending the immunization clinic of UATH, based on the average yearly register of the clinic.
The sample size determined used formula 15 for a single proportion
The contraceptive prevalence rate of 15% obtained from the Nigerian national demographic health surveywas used to obtain the sample size for the study (196). Additional 10% of the calculated size added to take care of non-response, bringing the total sample to 220 mothers 10.
The systematic sampling method was applied to draw a representative random sample. The immunization register served as the sample frame for every 9th mother. Subjects comprise women within 18-49 years with infants below 12months who gives consent and is willing to participate in the study. The study had a 90% return rate from 200 properly filed and returned questionnaires.
A structured questionnaire pretested and validated with reliability determined at Cronbach’s alpha 0.79 elicited responses on demographic variables, reproductive history, current and past contraceptive practice, barriers to use. The tool had a total of 48 items in 4 sections. The data collection was by self-administered questionnaire method by the researcher with the help of 1 trained assistant for one month.
After data cleaning, sorting and coding, the analysis was by Statistical Package for Social Sciences (SPSS) Version 25.0. Descriptive analysis and binary logistic regression to establish the relationship between variables with the p-value set at 5% level, thus p<0.05 is termed significant.
Ethical approval obtained from the review board of the UATH, the participants were educated, giving assurances of anonymity and confidentiality of their response and required to tick the consent form indicating consent for the study
RESULTS
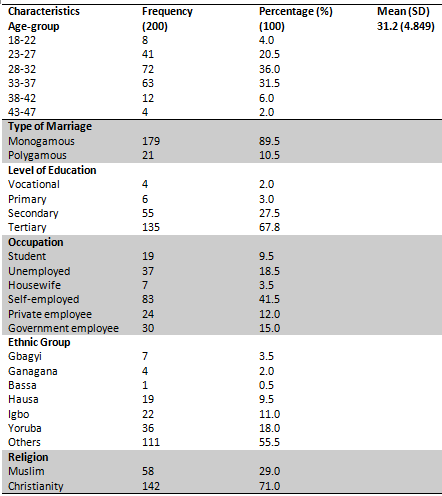
Table 1 presents the socio-demographic characteristics of the 200 respondents; the mothers had a mean age of 31.12. Two-third of the mothers (67.5%) were within the ages of 28-37years, many of the respondents were in a monogamous marriage (89.9%) above two-third had tertiary level of education (67.8%), while about 41% of the mothers were self-employed. 71.4% were Christians and over a quarter (28.6%) were Muslims.
Reproductive History of the Mothers attending UATH Abuja
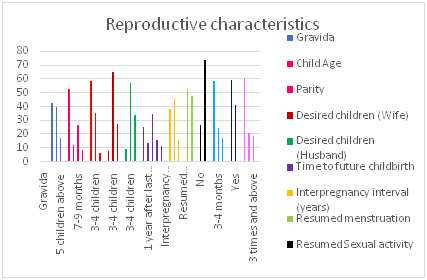
Figure 1 presents the reproductive history of the subjects. A majority (83.5%) have been pregnant between below four times while 17% have had above five pregnancies. About two-fifth (n=82) reported having a history of abortion, while four-fifth (81.7%) have had 1-2 abortions, and above half of the infant (53.3%) were 1-3months old, more than half (58.8%) of the subjects had 1-2 children while 6% had above 5.
On the number of children desired by the women, about two-third wanted 3-4 children, 27.5% desired above 5, whereas one-third (33.5%) reported their husbands desired above five children. One-fourth (25%) of the subject does not want to have more children while 34.5% would wait for two years after last delivery to have another child, close to two-thirds of the subjects gave an ideal inter-pregnancy interval.
Over half of the respondents (52.5%) indicated that they had not resumed their menstrual cycle after the last delivery while 73.5% have commenced sexual activity after last delivery, of which more than half (58.5%) commenced 1-2 months after delivery.
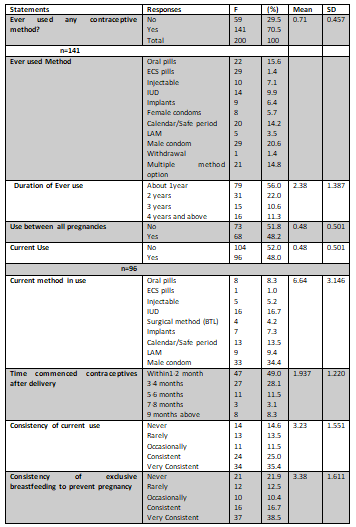
The analysis on table 4 revealed 70.5% (n=141) of the respondents had used a form of contraception in the past, over half (56%) used the method about one year whereas 51% did not use it between all pregnancies. Of the 200 mothers, less than half 48% are currently using a method of contraception.
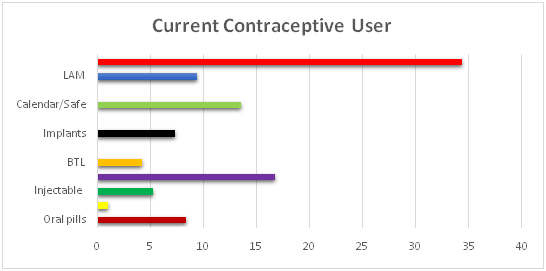
Of the 96 mothers currently using a method over one-third (34.4%) are using a condom, 16.7% use IUD, while 13.5% practice calendar/safe period. Almost half of the mothers (49%) started their method of contraception within 2months of delivery, three-fifth (60.4%) are consistent with practice while more than half (55.2%) consistently breastfeed to prevent pregnancy. Less than half of the mothers (47%) classified as having a good level of practice following analysis of their reported practice while over half (53%) have a poor level of practice.
Binary Logistic Regression Model showing association between contraceptive practice level with socio-demographic characteristics of mothers attending UATH
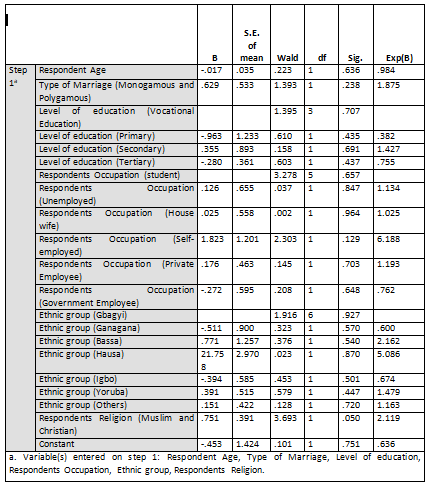
The Wald statistic has chi-square distribution which is significant at p<0.05. Therefore, any predictor variable that has p-value less than 0.05 is significant. Looking at the equation, it showed that the predictors except for religion are all not significantly predicting contraceptive practices among mothers in UATH since its p-value exceeded the 5% level of significance.
Only the predictor Respondent Religion of Muslim and Christian had a significant impact on contraceptive practices among mothers in UATH with p-value of 0.050. However, since the Respondents religion is significantly impacting on the use of contraceptives by women, the Exp (B) or the Odd ratio will be meaningful, implying that the Christian mothers have odds of using contraceptives that are 2.119 of the odds of the Muslims mothers. It means that the Christian respondents are more likely than Muslim mothers to use contraceptives since the Odd ratio of 2.119 is greater than 1 (2.119>1).
Consequently, rejecting the assertion there was no significant relationship between socio-demographic characteristics of mothers and their use of contraceptive.
Binary Logistic Regression Model showing the relationship between Contraceptive practice level and some reproductive characteristics of mothers attending UATH Abuja
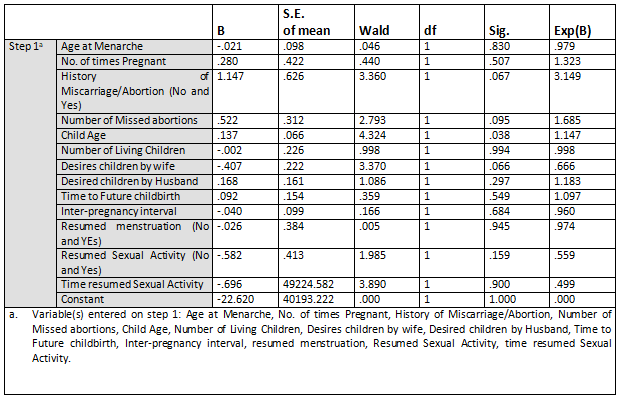
The Wald statistics results provided an index of the significance of each predictor variable in the equation. Wald statistics have chi-square distribution which is significant at p<0.05. Therefore, any predictor variable that has p-value less than 0.05 is significant. The equation showed that the only the predictor “age of the child” that has a significant impact on CP since the p-value of 0.038 is less than 0.05. Hence, one can conclude by saying that the age of the child is responsible for the use of contraceptives by mothers attending UATH.
All other variables are all not significantly predicting CP among mothers in UATH since its p-value is higher than 5% level of significance. However, History of Miscarriage/Abortion, Number of Missed abortions and Desires children by the wife are statistically significant at 0.1 (10% level of significance) since there p-value is less than 0.1.
Consequently, the assertion that there is no significant relationship between the reproductive characteristics of mothers and the use of contraceptive is not accepted.
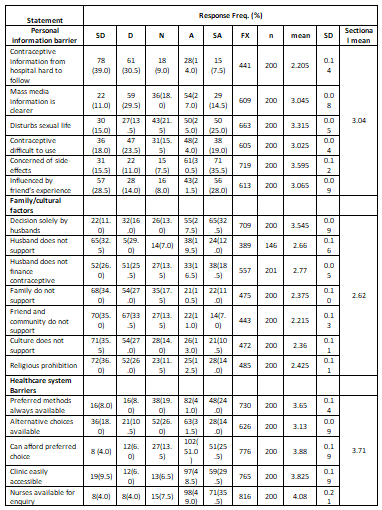
As seen from the percentage table above, one-fifth (21.5%) of the respondents agree that information provided in the clinic on contraceptives in the hospital is hard to follow, half (50%) indicated contraceptives disturbs their sexual life, two-third (66%) are concerned about side- effects, the experience of friends influenced nearly half. In contrast, over two-fifth (42%) are not.
From the sectional mean on the variable “Personal information barrier” (PIB) obtained is 3.04 (Neutral), this strongly suggests that the respondents are somewhat indifferent about the challenges associated with personal information on contraceptive use and practices.
Furthermore, on the barriers associated with family and cultural factors, over half (57.5%) of the mothers reported their husband takes contraceptive decisions, more than one-third (35%) do not get financial support from the husband. In comparison, 23.5% and 24.5% indicated they do not have cultural and religious support to use contraceptives. The sectional of 2.62 (neutral) suggest that the respondents are indecisive. Thus, making the barriers from family and culture are not too much a determinant of contraceptive use or practices.
However, 16% indicated preferred method was not always available; one-tenth (10%) could not afford preferred choice, family planning clinic was not accessible 15% subjects, and 28.5% cannot access alternative contraceptive choices. The sectional mean obtained from the variable “Health system barrier” (HSB) is 3.71 (Agree), implying that barriers associated with the health system strongly impact on the use of contraceptives by the respondents.
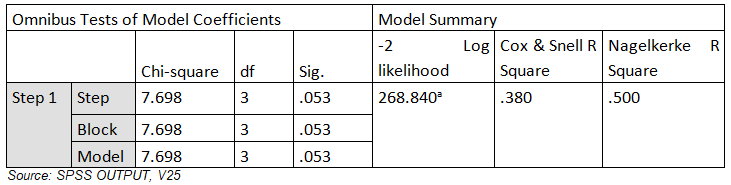
The analysis showed that logistic regression was significant (X2=7.698, df=3, p=0.053); this implies that PB, FCB, and HSB influenced the contraceptive practices (CP) at 5% level of significance. Nagelkerke R Square result revealed that 50% (0.500) of the variability in the contraceptive practices that was explained by PB, FCB, and The results in the model summary showed that the predictors used to predict contraceptive use by mothers are effective. Also, the result of the overall percentage accuracy value of 70.4% exceeded the standard limit of 56.6%, which implies that the logistic regression model was instrumental in the explanation of the CP and factors influencing it.
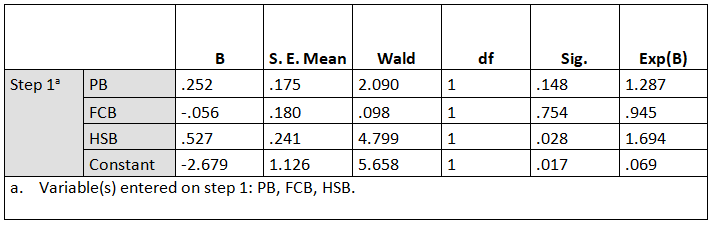
The Wald statistics results provided an index of the significance of each predictor variable in the equation. Wald statistic has chi-square distribution which is significant at p<0.05. The results showed that only HSB (X2=5.658, p<0.028), significantly predicted the CP. Other predictor variables in the model did not contribute significantly to CP (p>0.05), thereby rejecting the hypothesis.
DISCUSSION
The results showed that over 80% of the respondents were in the 23-37 age groups and had a mean age of 31, a standard deviation of 4.849. This result is similar to previous studies and another covering six states in the south of Nigeria12, 11, 16, 17. Reproductive activity is highest in this group with the heightened expectation for contraceptive usage 18.However, the mean age of respondents in Sudan appeared higher compared with lower age reported in this study 19.
There were more Christians (71.4%) in monogamous marriages (89.9%), over two-thirds (67.8%) had tertiary level of education whereas two-fifth are self-employed. The higher mean age and level of education shows more women are taking to education, thus delaying the age childbearing. Mothers in this study have a higher level of education compared to findings in various parts of Nigeria 20, 17,21. It confirms the rising educational attainment of women in the country as seen in the demographic health survey 10 .
Most mothers (94%) had below four children; this is higher compared to 59% in the Southeast but lower compared to 57.8% with above five children in Northwest Nigeria17,16 .The mean number of children is also lower compared to that obtained in Kenya and Malawi22,23 .The mean parity in this study is lower than the national total fertility rate of 5.5, and that of the north central zone of 5.3 signifying a downward reduction in childbirth in the zone 10.
The parity of the respondents seems to correspond with their desired number of children; this is a welcomed development when women begin to adopt a way of “living” and “thinking” that supports responsible decisions to promote their health and wellbeing. On the other hand, they might not have reached the saturation point to want to stop childbearing, thus providing evidence of contraceptive need.
While more than half of the respondents (52.5%) indicated that they had not resumed their menstrual cycle after the last delivery, 73.5% indicated they had started the sexual activity. The finding appears higher compared to 67.9% who resumed in 8 weeks in Kano-Nigeria, 65.1% in Ethiopia after two weeks but lower compared with 80% resuming in 2-3months without contraceptives in Malawi 21,22,24 .
Over half of the mothers are below three months postpartum, above half gave an ideal inter-pregnancy interval with a quarter have no intention for future childbirth while 61% wish to space for above 2years. The real need for contraception is for those who have no future intention and those needing to delay pregnancy.
Moreover, of 82 (41%), mothers with a history of abortion, almost two-third (61%) have had one abortion, nearly two-fifth (39%) reported 2-3 incidences, this finding is higher compared to a study where 24% had an unintended pregnancy, and 19.2% had a history of abortion 25. There is evidence of contraceptive usage gap. The implication is the increased pregnancy and abortion risk; this confirms the 16% cases of unwanted pregnancy reported in the same center is yet to receive the needed attention, and the figure is rising 4.
The analysis of results revealed that below half current users (47%) had right contraceptive practice level compared to above average (53%) with poor practice. Findings indicated that less than half the mothers (n=96, 48%) currently apply a method although almost three-quarter (n=141, 70.5%) have used a method of contraception in the past. This result is similar to that in Ethiopia and Ghana 14, 26 but higher compared to findings (45.8%) of Berta et al 24, howbeit one study in South-western Nigeria report higher percentage 20. This study’s subjects with good practice level contrast with 11% two reportedas only 22.9% are current users. Consistent contraceptive use complemented by exclusive breastfeeding increases practice level, benefits the mother, baby, family and the community 6, 25.
This research’s practice level (47%) is higher than the national average of 15% this could be explained by the setting; facility-based, urban-setting which might influence the use or intention to use a contraceptive. Observation during the period of the study showed that more women visited the family planning clinic after filling the questionnaire; the study served as a source of information and reminder for those who had forgotten.
The most common method used by the respondents is the condom (34.4%), though 42.7% use a modern method; one-fifth of the mothers use the natural method. The commonly used modern methods are IUD, oral pills and implants. Close to half of the mothers confirmed the use of condoms by their husbands which corresponds with the mother’s method (condom), a good observation that the men are participating in family planning. Attention should be paid proper use for maximum dual benefit. Some authors corroborate the results and that more women use the condom 17, 20.
The logistic regression analysis for contraceptive practice and all the social-demographic characteristics of the mothers was not significant, except for the respondent’s religion. This finding is consistent with studies in the north and west of Nigeria where religion, marriage and ethnicity showed association with contraceptive use16, 20.
It is noteworthy that only 18.6% of the cumulative reproductive characteristics of the mothers’ contraceptive use/practice. Only the predictor “child’s age” had a significant impact on contraceptive practices among mothers in UATH (p=0.038). One-fourth with infants less than six months are current users, more (37.7%) are not. It is conspicuous that those with younger children use long-acting reversible contraceptive and four mothers had a bilateral tubal ligation. These methods offer the highest protection against unplanned pregnancy in addition to reduced menstrual bleed and cancer protection.
On the other hand, history of Miscarriage/Abortion, Number of Missed abortions and desired children by the wife are statistically significant at 0.1 (10% level of significance).
Children desired by wife had a significant relationship with contraceptive use (x2=3.370, p<=0.066). More mothers have an average of 3 children and most (with their husbands) desire 3-4 children, this contrast with a Malawian study with more women desiring more than five children 22. A study in Nigeria confirms the independence of parity with use; a decline in fertility could be responsible for the trend. The desire for fewer children in this study shows an unprecedented decline from the previous findings 5.7 between 2003-2008, 5.5 in 2014 (5.3 in Abuja) 10.
Comparatively, history and number of abortions revealed a statistical relationship with contraceptive use (p=0.067 and p=0.095) Signifying as the history of abortion increased, a corresponding increase in the number of abortions and contraceptive usage occurs. Howbeit, over one-third mothers with a history of abortion are current users. Women do not have to experience an abortion before adopting contraceptives.
Two-third (66%) of the respondents confirmed they had fear concerning side-effects, about half agreed to been influenced by experiences of friends and neighbors. Fear of side-effects, as reported in literature across Nigeria, ranged from 14.6% in Western to 50.3% in the South and 58.8% in the Northern region16,17,20.On the contrary, this population expressed more fears and a better understanding of contraceptives compared to those references above. About 43%respondents in Ethiopia indicated fear of side-effects prevent their use of contraceptives, but a more recent study in Ethiopia presented lower results 24% and 34.6% in Egypt 24.
Concerns about side-effects could be related to contraceptive knowledge, level of education and understanding of the information given by the healthcare practitioner. Albeit 71% affirmed they understood contraceptive information given at the clinic. A study reported the opposite; the subjects had a less contraceptive phobia. The mothers have a higher level of education but seem to be more apprehensive using contraceptives 14.
About two-third pinpoint, the decisions are taken solely by their husbands; over a third had financial support for its use while 21.5% of family members do not support contraceptive use. In like manner, 33.3% of participants in Abakalike, 1724% in Ethiopia, 24 25% in Sudan 19 indicated a lack of spousal consent as a barrier. Howbeit 81.9% of respondents in Ghana got financial support from their husbands, while 5.2% think the contraceptive decision should lie with the husband.[26]Though three-quarter of the mothers reported they could afford contraceptives, one-third are not empowered (unemployed, house-wife and student), when the husbands do not finance contraceptive use, it is a subtle barrier that is downplayed by the respondents.
Over one-fifth and 26.5% of the mothers agree that their culture and religion prohibit the use of contraceptives and religion determined (p=0.050) contraceptive use results are close to this study with 18% and 15% having cultural and religious barriers. However, a higher report 39% and 50.6% have reported for the socio-cultural and religious barrier. Impliedly, religion, community, and cultural affiliations determine the reproductive activity of mothers.
The majority (96%) think the HSB was not strong enough to prevent the use of contraceptive. Unavailability of choice with having to return for refill by of the participants is a significant constraint. Same was reported in a facility-based study, while adding information gap and provider attitude as a challenge. Though health providers may give required information during health talk, the ability to elicit responses about clarity may be a crucial factor preventing uptake. Some participants identified problems of having to interact with the source of information, the pattern of presentation and health literacy as a hindrance13. Therefore, it is not surprising as this study population were reluctant in identifying health professionals as a barrier been that the researcher is one of them.
In summary, the respondents appear indifferent about the challenges associated with personal information on contraceptive use and practices. The sectional mean reflected as neutral (3.04), while the mothers appeared undeceive regarding family/cultural factors (2.62). However, the sectional mean obtained from the variable “Health system barrier” is 3.71 (Agree), implying that barriers associated with health system strongly impacts and determine the use of contraceptives by the respondents. Report of many authors confirms this finding 13, 26. To conclude, the regression analysis confirmed HSB strongly determine contraceptive use (X2=5.658, p<0.028).Other predictor variables in the model did not contribute significantly to CP (p>0.05), thereby rejecting the hypothesis.
Ethical Clearance: Ethical clearance has obtained from University of Abuja, Teaching hospital, Nigeria, West Africa, to conduct this study with reference number: UATH/HREC/PR/2019/005,Dated 20/08/2019.
Conflicts of Interest
The author declares that there is no competing interest on conduct of this study and in publishing this article.
Fund for the study: This is self-funded study.
CONCLUSION
This research has shown that 48% (96) of the women are currently using a form of family planning out of which only 41.7% use modern contraceptives and 19.1% follow the natural method. The most common method used by women is the condom.
Majority of the mothers reported being concerned about side-effects but were not bothered by the concerns of family and neighbors; they confirmed understanding and knowledge of contraceptive education given in the hospital. The mothers were indifferent on personal information barriers; howbeit, the health system strongly impact on the use of contraceptives by the respondents.
The contraceptive practice is not dependent on any of the social characteristics of the mothers except for religion; Child’s-age predicted contraceptive use; an important feature is that women with younger children use long-acting contraceptives. Therefore, encouraging women early in postpartum will likely produce more compliant contraceptive users.
Practice Implications
Healthcare providers have to provide contraceptive education at every contact with all women of reproductive age. Nurses must avoid judging the level of contraceptive knowledge based on the educational attainment of their client. Nurses must elicit the method-specific knowledge from each client during counseling in order to give accurate information, dispel misconception and advice on how to seek help for side effects. To achieve this, health workers must take part in training and retraining to remain competent providers.
The reduced fertility desires recorded in this study is a welcomed development, effort must be intensified on the part of the government and health providers to sustain it with more facilities for family planning and trained staff.
Limitations of the study: The researcher observed the following limitations to the study:
This study set does not allow sampling of more indigenous mothers in the city. The researcher recommends future study with a larger sample from various settings to increase its generalizability.
Agida T., Akaba G., Ekele B. and Adebayo F (2016). ‘Unintended pregnancy among antenatal women in a tertiary hospital in North Central Nigeria’, Niger Medical Journal; 57(6):334-338.
- Agida T., Akaba G., Ekele B. and Adebayo F (2016). ‘Unintended pregnancy among antenatal women in a tertiary hospital in North Central Nigeria’, Niger Medical Journal; 57(6):334-338.
- Saleh, S., Raji, M., Oche, M., Tunau, K and Kaoje, A (2018).‘Socio-demographic Factors Associated with Knowledge and Uptake of Family Planning Among Women of Reproductive Age in a Rural Community of Abuja, Nigeria’, Journal of Sains Kesihatan Malaysia 16(1): 71-79.
- Onuorah, W and Jamda, A (2017). ‘Knowledge and Beliefs Regarding Contraception among Married Women in Gwagwalada, Abuja,’Nigeria Journal of Advances in Medicine and Medical Research 23(12): 1-12.
- Yidana, A and Sharif, A (2018). ‘Family Planning Use Among Women Attending a Health Care Facility in Rural Ghana”, Central African Journal of Public Health, 4(4), pp. 119-124.
- Demie, T., Demissew, T., Huluka, T., Workineh, F., Libanos, H (2018). ‘Postpartum Family Planning Utilization among Postpartum Women in Public Health Institutions of Debre Berhan Town, Ethiopia’, Journal of Women’s Health Care 7: 426.
- Mohammed-Durosinlorun, A., Idris, Z., Adze, J., Bature, S., Mohammed, C., Taingson, M., Abubakar, A., Avidime, S., Airede, L and Onwuafua, P. (2016). ‘A quantitative survey on potential barriers to the use of modern contraception among married women of high parity attending an antenatal clinic in Kaduna, Northern Nigeria’, Archives of Medicine and Surgery;1:30-4.
- Esike, C., Anozie, O., Ani, M., Ekwedigwe, K., Onyebuchi, A. and Ezeonu P. (2017). ‘Barriers to family planning acceptance in Abakaliki, Nigeria. Tropical Journal of Obstetrics and Gynaecology, 34:212-7.
- Eluwa, G., Atamewalen, R., Odogwu, K.,& Ahonsi, B. (2016). Success Providing Postpartum Intrauterine Devices in Private-Sector Health Care Facilities in Nigeria: Factors Associated with Uptake’, Global health, science and practice, 4(2), 276-283.
- Abdalla, A and Ahmmed, E (2017). ‘Evaluate Use and Barriers to Accessing
IJMAES, Vol 6 (4), 836-853, December 2020 ISSN: 2455-0159
International Journal of Medical and Exercise Science |2020; 6 (4) Page 852
Family Planning Services among Reproductive Age Women in the White Nile, Rural Districts, Sudan’, Health Science Journal,11(6): 531. - Durowade K., Omokanye, L., Elegbede, O., Adetokunbo, S., Olomofe, C., Ajiboye, A., Adeniyi, M., Sanni, T (2017). ‘Barriers to Contraceptive Uptake among Women of Reproductive Age in a Semi-Urban Community of Ekiti State, Southwest Nigeria’, Ethiopian Journal of Health Science, 27(1):121.
- Iliyasu Z., Galadanci, H., Danlami, K., Salihu, H and Aliyu, M (2018). ‘Correlates of Postpartum Sexual Activity and Contraceptive Use in Kano, Northern NigeriaAfrican Journal of Reproductive Health March; 22(1):103.
- Bwazi, C., Maluwa, A., Chimwaza, A. and Pindani, M. (2014). ‘Utilization of Postpartum Family Planning Services between Six and Twelve Months of Delivery at Ntchisi District Hospital, Malawi’, Health, 6, 1724-1737.
- Ochako, R., Mbondo, M., Aloo, S., Kaimenyi, S., Thompson, R., Temmerman, M and Kays, M (2015). ‘Barriers to modern contraceptive methods uptake among young women in Kenya: a qualitative study’, BMC Public Health, 15:118.
- Berta, M., Feleke, A., Abate, T., Worku, T., and Gebrecherkos, T. (2018). ‘Utilization and Associated Factors of Modern Contraceptives During Extended Postpartum Period among Women Who Gave Birth in the Last 12 Months in Gondar Town, Northwest Ethiopia’, Ethiopian Journal of health sciences, 28(2), 207–216.
- Tebeje B and Workneh D (2017). ‘Prevalence, Perceptions and Factors Contributing to Long-Acting Reversible Contraception Use among Family Planning Clients, Jimma Town, Oromiya Region, South-West Ethiopia. Journal of Women’s Health Care 6: 351.
- Kaydor, V., Adeoye, I., Olowolafe, T. and Adekunle, A. (2018). “Barriers to acceptance of post-partum family planning among women in Montserrado County, Liberia”, The Nigerian postgraduate medical Journal, 25(3), pp. 143-148.
- Jarvis, L., Wickstrom, J., Vance, G and Gausman, J (2018). ‘Quality and Cost Interventions during the Extended Perinatal Period to Increase Family Planning Use in Kinshasa, DRC: Results from an Initial Study, Global Health: Science and Practice, 6(3).
- Onifade, O., Ogungboye, O Adigun, J., Abikoye, A., Abiola O., Aliyu, S (2017). ‘Socio-Cultural Factors Influencing Choice of Bilateral Tubal Ligation Among Women Attending University of Ilorin Teaching Hospital’, KIU Journal of Social Sciences, ISSN: 1996902-3; 3(1): 37-46.
- Mohammed, A and Bhola, K (2019). ‘Challenges and prospects of contraceptives use among women attending family planning services in Yobe State, Nigeria’,World Scientific News, 122, 122-132.
- Ayanore, M., Pavlova, M., Groot, W. (2017). ‘Context-specific Factors and Contraceptive Use: A Mixed Method Study among Women, Men and Health Providers in a Rural Ghanaian District. African Journal of Reproductive Health, 21(2):81-95.
- Dona, A., Abera, M., Alemu, T., and Hawaria, D. (2018). ‘Timely initiation of postpartum contraceptive utilization and associated factors among women of child bearing age in Aroressa District, Southern Ethiopia: a community based cross-sectional study’, BMC public health, 18(1), 1100.
- Jalang’o, R., Thuita, F., Barasa, S. O., and Njoroge, P. (2017). ‘Determinants of contraceptive use among postpartum women in a county hospital in rural Kenya’, BMC Public health, 17(1), 604.
- Nigatu et al. (2016Nigatu, D., and Segni M (2016). ‘Barriers to Contraceptive Use Among Child Bearing Women in Ambo Town, West Shewa Zone, Oromia Regional State, Ethiopia’, Gynecology Obstetrics (Sunnyvale) 6: 352.
- Elsayda et al. 2018 Dr, Elsayda, H., Dr Mirfat, M and Dr Esraa, M (2018). ‘Factors Influencing Utilization of contraception among Women in Port Said City’, Journal of Nursing and Health Science (IOSR-JNHS); 7(5) PP 53-63.
- James et al. 2018James, S., Toombs, M., Brodribb. W (2018). ‘Barriers and enablers to postpartum contraception among Aboriginal Australian women: factors influencing contraceptive decisions’, Australian Journal of Primary Health, Research 24, 241–247.
- Unumeri, G., Ishakua, S., Ahonsi, B and Oginnia, A (2015). Contraceptive Use and Its Socio-economic Determinants among Women in North-East and North-West Regions of Nigeria: A Comparative Analysis’, African Population Studies, 29(2), 2015:1851.
Citation:
Ochala Ejura Jennifer, Rauf Ibrahim, Samsiah Mat, Syed Ali Gulab Jan (2020). Postpartum contraceptive practice and barriers to its use among mothers from a tertiary hospital in Abuja, Nigeria , ijmaes; 6 (4); 836-853.

Leave a Reply