An Analysis on the effect of Buteyko Breathing and relaxed postures over the chest exapnsion of asthmatic collegiate population- An experimental study
Gladies Kamalam. S 1, Srividya. G2, Andrews Milton. J3
Corresponding Author:
1Associate Professor, Bethany Navajeevan College of Physiotherapy, Kerala, India. Mail id: mail2drsgk@gmail.com
Co Authors:
2 Research Guide, Department of PMR, Annamalai University, Tamilnadu, India.
3 Research Co- Guide, Bethany Navajeevan College of Physiotherapy, Kerala, India.
ABSTRACT
Background: Over ages; bronchial asthma and its adverse physiological, psychological impacts upon varied group of age, people, and health remains a searchable quest in its depth. Behaviour modification as an emerging outlook of Physical therapy helps to exhibit positive changes in this broad spectrum of asthma. This study aimed to identify the possible potential factors to improve chest expansion by analysing the effect of buteyko breathing and relaxed postures.
Methods: Experimental study design; 20 patients of the age group 17-19 years were selected using simple random sampling method. Group A; consisting 10 patients were advocated buteyko relaxation training. Group B; consisting of 10 patients were advocated relaxed postures along with the conventional asthma management. Stop watch, nose clip, inch tape,pediatric asthma quality of life questionnaire [PAQLQ] were used as the operational tools. Paired and Unpaired “t” testing was used to analyze the pre- test and the post- test values after a period of 6 months.
Results: Analysis of the peak expiratory flow rate and the quality of life over Group “A” and Group “B” at 0.05% level of significance showed positive results for Group “A” when compared with the ‘t’ value.
Conclusion: The findings support the multidimensional positive effects of behavior modification over the physiological and psychological parameters that lead to the onset of bronchial asthma.
Keywords: Bronchial asthma, behavior modification, buteyko breathing, relaxed postures, peadiatric asthma quality of life questionnaire.
Received on 3rd May 2019, Revised on 4th June 2019, Accepted on 8th June 2019
INTRODUCTION
Bronchial asthma is related as a variant of chronic non- specific lung disease [CNSLD] as well as chronic obstructive pulmonary disease [COPD]. In the recent times, there has been an increasing awareness and emphasis on the functional, psycho-social aspects of health of the patients and their quality of life. Long term e5ffects focuses on the importance of quality of life and its valid implications on the positive outcomes of respiratory rehabilitation4.
Behavior modification is considered to be a key reliever from a rehabilitation perspective. Behavior modification is a form of respiratory adaption based upon the improvement in psychological facilitators of health. Modification in breathing and behavior may be adapted by a subject during marked respiratory discomfort. Even in healthy subjects, the negative implications of psychological risk factors, promotes uncomfortable perception of resistance to airflow which may alert the subject to increase respiratory muscle force or to switch to mouth breathing which is a common clinical sign seen in asthmatics5,1.
Such risk factors may become subconscious habits. The effect of thoughts and emotions on breathing has been studied by experimental psychologists using non invasive respiratory monitoring techniques. There exists a strong correlation between respiratory psychophysiology and behaviour modification. Golla and Antonovitch (1929) found that there were normal subjects who had habitually irregular breathing patterns and that these differences were related to the types of imagery used in the subjects.
Recent statistics say that asthma is found to occur more frequently in children with approximately one in five children suffering from the condition. It has been the primary cause of class absences, and the third leading cause of hospitalizations in the mean age of 15 – 20 years with boys more frequently affected than girls. The World health organization in 2007 stated that; 300 million people worldwide suffer from asthma.
Minnesto department of health, Asthma programme, 2004; accounts for 14 million lost school days annually due to asthma were reported. MMWR, Surveillance National Health Statistics 2003, reported 6.3million children under 18 have asthma. Despite significant improvements for disease control by the development of different drugs; its world prevalence is increasing worldwide which poses a continuous threat in the health sector. Impact of the physical and physiological changes experienced during the attacks have adverse effects on the psychological well being of the individual leading to reduced health status, increased stress, lack of relaxation etc2,3,4.
The International Study of Asthma and Allergies in Childhood (ISSAC) programme is currently the only global study of pediatric asthma and allergy currently in existence focusing on the coping skills, activities of daily living and play time of the affected children periodically decreased by attacks of asthma. Buteyko’s theory put forward by Prof. Konstantin Pavlovich Buteyko (1923-2003); a Russian doctor, says that because hyperventilation causes asthma; a reduction in over-breathing results in a reduction of the severity of asthma and therefore the need for medication. It was indeed proven by the trials that this technique has no side effects and can be certainly used as an adjunct in treating asthma (Published by American Thoracic Society on May23, 2006).
Opat A.J et al., in 2000 stated that; Buteyko breathing technique shows a modest improvement in quality of life and reduction in bronchodilator use. Buteyko breathing method aids in relaxation and helps in consciously reducing the breathing rate and breathing volume. This involves altering the pattern of breathing which slows down the respiratory rate. The implication of Buteyko method has its emphasis on reducing the onset of asthmatic symptoms, decreasing the intake of reliever medications, improving the quality of life and exercise endurance. Psychology in the Schools, Nov 2003, stated that; Relaxation interventions improved FEV1 and decreased anxiety among school going children6,7.
As seen in studies, both anxiety and depression are associated with activation of the hypothalamic–pituitary–adrenal (HPA) axis and increased systemic inflammatory responses that could be responsible for an increased risk of exacerbations. Physiological deregulation (e.g., activation of the SNS and HPA axis) induced by chronic psychological stress may weaken immune function and potentially increase vulnerability to respiratory infections and COPD exacerbations. Patients with anxiety and depression often suffer from low self- confidence or self-efficacy, which may lead to worse disease-related coping and poor self- care behaviors.
Loew TH, et al in 1996; stated that; Functional relaxation reduces acute airway obstruction and is used in the relief of asthma. Browler SD, et al in 1998 stated that Buteyko breathing technique efficiates significant reduction in hyperventilation and better quality of life was observed in the patients without objective changes in measures of airway calibre9.
Relaxation both physiologically and physically is essential during the episodes of asthma. Conventional relaxation postures along with deep diaphragmatic breathing exercises are found to provide a little ease in reducing the exacerbation and the anxiety caused due to the attack. Tanka.Y et al in 1998 stated that; Nasal breathing protects the airways by humidifying, warming and cleaning the air entering the lungs. C.Lachman, et al in 2009 stated that; Functional relaxation has positive effects on asthma.
The overall goal of asthma management in health care is: to maintain normal activity levels, to maintain normal pulmonary function, to prevent chronic symptoms and recurrent exacerbations by assisting the child in living as normal and happy a life as possible4,16. Thus this study helps to analyze the effects of buteyko relaxation technique on the quality of life among children with an acute episode of asthma.
Need For The Study: Buteyko relaxation technique has been found to be an effective basic, non-invasive, affordable, and portable adjunct with no side-effects. This technique creates sense to try it first to alleviate symptoms exhibited during asthma. The main aim behind is to help the people help themselves by using a natural solution. Results show that this is a better choice of complimentary treatment for responsibly managing respiratory health care, rather than condoning a drug dependent future.
Objectives: To find out the effect of relaxed postures in collegiate population with acute asthma.To find out the effect of buteyko breathing in collegiate population with acute asthma.To compare the effects of relaxed postures and buteyko breathing technique in s collegiate population with acute asthma.
Hypothesis:
Alternate hypothesis: There will be significant difference in Chest expansion between relaxed postures and buteyko breathing pattern technique in children with an acute episode of asthma.
Null hypothesis: There will be no significant difference in Chest expansion between relaxed postures and buteyko breathing pattern technique in children with an acute episode of asthma.
METHODOLOGY
Study Design: A two group, pre test and post test experimental study design. Study Setting; Out Patient Department. Study Duration: 6 months. Subjects: The sample population involved in this study. GROUP A – Experimental group. GROUP B – Control group17, 18.
Selection Criteria
Inclusive criteria: A total of 20 patients were included for the study using a simple random sampling method. Patients with asthmaof both sexes were included with Age group between 17-19 years.
Exclusive criteria: Patient with status asthmaticus. Patient with cardiothoracic, orthopedics, neurological problems.Patient with skin, peripheral vascular disorder and infectious diseases were excluded from this study.
Operational Tools: Stop watch, Nose clip, Inch tape, Pediatric asthma quality of life questionnaire [PAQLQ].
Statistical Tool
Paired‘t’ test was used to compare pre test and post test values of the same group. Unpaired‘t’ test was used to compare the pre test and post test values of Group A and Group B.
Administration Of The Technique: A total of 20 patients were taken by Simple Random Sampling and were divided into two groups of 10 each. A written consent form was obtained from the patients and from the parents’ of the selected patients and was divided into group A and group B.
Group A – underwent buteyko relaxation technique [A Ukrainian method of physical therapy practiced for the treatment of asthma involving a series of breathing exercises that focus on nasal breathing, breath holding and relaxation].
Group B – Underwent conventional relaxed postures of asthma management. The pre test values were taken to measure Chest Expansion using an inch tape and Quality Of Life using the Pediatric Asthma Quality Of Life Questionnaire (PAQLQ). All the patients of group A had one orientation session to buteyko technique before implementation. The patients assigned in group B were encouraged to follow the normally adapted relaxation postures with deep diaphragmatic breathing. Both the groups underwent the usage of nebulizers.
Patients in group A were asked to practice the control pause method of buteyko technique which helps to control over breathing by breath-holding. After the normal exhalation the patients’ were asked to hold the nose between thumb and fingers until the urge to breathe again is felt. A nose clip was used to hold up the nose. The number of seconds elapsed between holding the nose and releasing is noted which marks the control pause time. The group B patients adapted the general relaxation posture during the episodes of asthma as a conservative mean.
RESULT
Each session of the exercise program lasted for 20 minutes. Each group had two sessions each day in an eight day period for a duration of six months. The outcome measures analyzed were chest expansion using an inch tape and quality of life using the Pediatric Asthma Quality Of Life Questionnaire (PAQLQ). The post test values were taken on both groups after 6 months to measure the impact on chest expansion and Quality Of Life using the Pediatric Asthma Quality Of Life Questionnaire (PAQLQ).
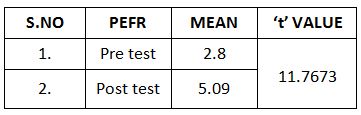
This table shows the analysis of chest expansion on Paired‘t’ test. The‘t’ test value for Group A was 11.7673 at 0.05% level of significance, which was greater than the tabulated ‘t’ value 2.201. The result shows that there was marked improvement in Chest expansion between pre test and post test values of Group A.
This table shows the analysis of chest expansion on Paired ‘t’ test. The ‘t’ test value for Group A was 11.7673 at 0.05% level of significance, which was greater than the tabulated‘t’ value 2.201. The result shows that there was marked improvement in Chest expansion between pre test and post test values of Group A.
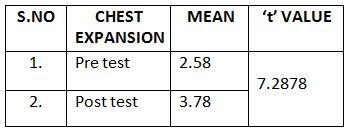
This table shows the analysis of Chest expansion on Paired ‘t’ test. The‘t’ test value for Group B was 7.2878 at 0.05% level of significance, which was greater than the tabulated ‘t’ value 2.365. The result shows that there was marked improvement in chest expansion chest expansion between pre test and post test values of Group B.
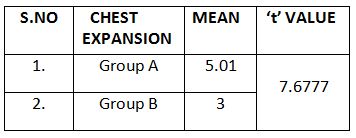
This table shows the analysis of chest expansion on unpaired‘t’ test. The‘t’ value for Unpaired ‘t’ test was 7.6777 at 0.05% level of significance, which was greater than the tabulated ‘t’ value 2.365. The result shows that there was marked improvement in chest expansion of patients in Group A than in Group B. This shows that the study accepts the Alternate hypothesis and rejects the Null hypothesis.
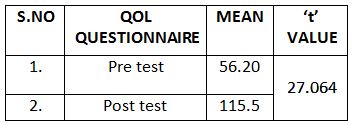
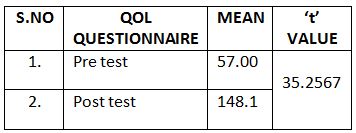
This table shows the analysis of Quality of life on Paired‘t’ test .The ‘t’ value for Group A was 2.584 at 0.05% level of significance, which was greater than the tabulated ‘t’ value 1.833. The result shows that there was marked improvement in Quality of life between pre test and post test values of group A.
This table shows the analysis of Quality of life on Paired‘t’ test. The‘t’ value for Group B was 2.191 at 0.05% level of significance, which was greater than the tabulated ‘t’ value 1.833. The result shows that there was marked improvement in Quality of life between pre test and post test values of Group B.
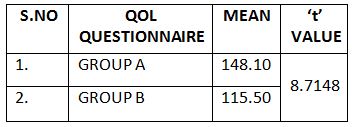
This table shows the analysis of Quality of life on unpaired ‘t’ test. The ‘t’ value Group A and Group B was 3.741 at 0.05% level of significance, which was greater than the tabulated ‘t’ value 1.734. The result shows that there was marked improvement in Quality of life of patients in Group A than in Group B. This shows that the study accepts the Alternate hypothesis and rejects the Null hypothesis.
DISCUSSION
The study was made to analyze the effect of buteyko breathing technique on the quality of life of asthmatic population. The study’s functional parameters for measurement were chest expansion, and Pediatric asthma quality of life questionnaire [PAQLQ].
Bowler.SD et al in Dec1998 stated that Buteyko Breathing Technique is a new trend towards better quality of life in asthmatic children. The British Thoracic Society in May 2008 has upgraded the Buteyko method in to “B” classification. No other complementary therapy has been endorsed by this body to such higher grades for asthma 12, 13.
Dr.Robert Cowie; who is the resident respirologist of foothills hospital in Calgary and a Researcher on the Buteyko Breathing Technique during his trails in the time period Oct 2004-Apirl 2005 said that; ʻʻI have been astonished and also very pleased with the excellent result. There is no disruption of their life at all by their disease, normal activities, not waking at night; not needing to use any reliever medications. It’s just great, 78% controls is about as good as anyone has got in any study of asthma”. This proves that the buteyko technique is more effective when compared to any other conventional respiratory adjuncts.
Interpretation of results for measuring the significance of buteyko breathing technique over the conventional method at 0.05% level of significance through the paired ‘t’ test that the ‘t’ value in Group A is 11.7673 which is widely significant than the ‘t’ value in Group B which is 7.2878. Both the values are greater than the tabulated ‘t’ value which is 2.365.
Mc. Hugh P. et al in Jan 2004 said that buteyko breathing technique is a safe and efficacious asthma management technique which supports the interpretation of results while analyzed at 0.05%of level of significance proving that the unpaired ‘t’ test value was 7.6777which is greater than the tabulated ‘t’ value.
American Family Physicians Statement (2000), have proved that the patients trained with Buteyko training has showed a significant reduction in the dysponea symptoms at rest, increased oxygen consumption and total work capacity which deflate the lungs and allow it to return to the passive Functional Residual Capacity (FRC) and showed a marked improvement in the Quality of life in patients with bronchial asthma as this simulates an endurance training.
The administration of Pediatric asthma quality of life questionnaire
[PAQLQ] to analyze the anxiety and emotional levels of the children
was found to be beneficial in improving the Quality of life in children. Juniper
EF et al in 1999 said that the Pediatric asthma quality of life questionnaire
[PAQLQ] has good measurement properties and is valid both as an evaluative and
discriminative instrument. It provides information to conventional clinical
outcomes11, 12.
Hallini M, et al, in 2008 June stated that; enforced mouth breathing decreases lung function in mild asthmatics. Cowie RL, et al., in 2008 May stated that; Buteyko technique can be used as an adjunct to conventional management of asthma and reduced the inhalation of corticosteroids. Ajay Bishop et al., in 2006 stated that; Nasal breathing increases the end tidal carbon dioxide in people with asthma. McHugh P, et al., in 2003 December stated that; Buteyko breathing technique for asthma is a safe and efficacious asthma management technique.
Li – Chi. Chiang, et al in 2009 Aug. stated that; a combination of self management and relaxation – breathing training can reduce anxiety, thus improving asthmatics’ children health. H. Mussafi et al in 2001 stated that; Pediatric asthma quality of life questionnaire [PAQLQ] provides additional insight to physicians’ assessment in routine asthma care.The above studies for assessing the quality of life proves to be widely significant in Group A who were administered with buteyko relaxation technique than the Group B patients, who were administered the conventional relaxation postures 10.
Interpretation of the results for measuring the significance of Pediatric asthma quality of life questionnaire [PAQLQ] at 0.05% level of significance says that through the paired ‘t’ test, the ‘t’ value in Group A is 35.2567 , which is widely significant than the ‘t’ value in Group B which is 27.0635. Both the values are greater than the tabulated ‘t’ value which is 1.833.
Analysis of the data show that the ‘t’ value in the unpaired t test between Group A and Group B is 8.7148 which is greater than the tabulated ‘t’ value 2.365 at 0.05% level of significance. Elizabeth Scott et al in 2005 stated that; Relaxation response reduces the constant state of physiological arousal over perceived threats in times if chronic stress as in repeated asthma attacks19.
Thus the study gives a strong data support that the buteyko breathing technique improves the chest expansion and quality of life in children with an episode of acute asthma. This is a marked improvement in rising up the quality of life and decreasing the symptoms of asthma; thereby ultimately fulfilling the goal to asthmatic management. This will be an important advance in the direction of the promising Predictive, Personalized, Preventive, and Participatory (P4) medicine model.
Physiotherapy Implications: Buteyko Breathing Technique is beneficial because it: Normalizes breathing, Has no side-effects, Increases the physical fitness and quality of life, Improves the psychological confidence, Reduces the anxiety levels about physical activity, Reduces the symptoms of asthma,Reduces the use of relieving inhaler medications12, 14, 16.
CONCLUSION
Analysis of the study concludes that buteyko breathing technique is most effective than the conventionally adapted relaxation postures during an episode of asthma. This study supports the alternate hypothesis saying that buteyko breathing training helps to normalize breathing.
No one who has asthma breathes correctly: Exercises result in a gradual reduction in the overall intake and output of breath. Oxygen levels remain optimal as with normal rate of breathing where the oxygen levels are 98% but what does change is the levels of carbon- dioxide. This gas is produced in the body and serves to keep the airways open in improving oxygen absorption.
Limitations and Recommendations: Certain factors such as nutritional factors, psychological status would not be controlled during the period of study. Similar study can be done with other respiratory disease such as bronchiectasis, exercise induced asthma and deconditioning elderly patients. The impact of this study on other rationales affecting the respiratory physiology could be considered.
REFERENCES
- Killian K.J., P. Leblanc, D.H. Martin, E. Summers, N.L. Jones, and E.J.M. Campbell (1992). Exercise capacity and ventilatory, circulatory, and symptom limitation in patients with chronic airflow limitation. Am. Rev. Respir Dis. 146 (4):935-940.
- Knudson R J, Slatin RC, Lebowitz MD, Burrows B. (1976). The Maximal Expiratory Flow Volume Curve: Normal Standards, Variability and Effects of Age. Am. Rev. Respir. Dis 113(5):587-600.
- Goldman, H. I., and M. R. Becklake (1959). Respiratory function tests: normal values at median altitudes and the prediction of normal results. Am. Rev. Tuberc. 79(4) :454–467
- Lacasse Y, Wong E, Guyatt G H, King D, Cook D J, Goldstein R S.(1996). Meta- analysis of respiratory rehabilitation in chronic obstructive pulmonary disease. Lancet; 348 (9035): 1115-1119.
- American Thoracic Society (1987). Standards for the diagnosis and care of patients with chronic obstructive pulmonary disease (COPD) and asthma. Am Rev Respir Dis; 136 (1): 225- 44.
- Susan Mayor (2007). Breathing and relaxation technique cut asthma symptoms by one third Bri. Med. Jou. ; 335 (7611) : 119.
- Holloway EA, West RJ. (2007). integrated breathing and relaxation training (the Papworth method) for adults with asthma in primary care: a randomised controlled trial. Thorax, 62(12):1039-42.
- Elizabeth A Holloway, Felix SF Ram. (2004). Breathing exercises for asthma. Cochraine Database of Systematic Reviews.
- Ernst E. (2000). Breathing techniques- adjunctive treatment modalities for asthma: A systematic review, European Respiratory Journal.15 (5); 969- 972.
- Juniper EF, et al. (1996). Measuring quality of life in children with astma, Qual. Life Res; 5(1): 35- 46.
- William d mc cardle (1996). Exercise Physiology, 4th Edition, A Wolters Kluwer Company, Baltimori Maryland.
- Donna frownfelter, PT, Dpumat, (2006). Cardiovascular and Pulmonary Physical Therapy, 4th Edition, Mosby Elsevier Company.
- William e Deturk, PT, Phd. (2010).Cardiovascular and Pulmonary Physical Therapy.2nd edition,Mc Graw-Hill Publication.
- Rob Hebert, BAppsc, Mappsc, PhD, (2005). Practical Evidence Based Physiotherapy, Elsevier, USA
- Leon Chaitow, ND, DO, (2002). Multi Disciplinary Approaches To Breathing Patterns Disorders, Churchill Livingston.
- Alfred P. Fishman (1995). Pulmonary Rehabilitation, Marcel Delrke, Inc NewYork, USA.
- C.R. Kothari, (2001). ‘Research Methodology’, Vishwa Prakasam Pulications, New Delhi.
- P.S.S. Sundar Rao and J. Richard, (2001). Introduction to Biostatistics, 3rd edition, Prentice Hall of India,
- ACSM’S (2001). Guidelines for Exercise Testing and Prescriptions, 6th edition, Lippincott Williams and Wilkins.
Citation:
S. Gladies kamalam, G. Srividya, J. Andrews Milton (2019). An analysis on the effect of Buteyko breathing and relaxed postures over the chest exapnsion of asthmatic collegiate population – An experimental study, ijmaes, 5(2), 567-575.